August 04, 2025
4 min read
Key takeaways:
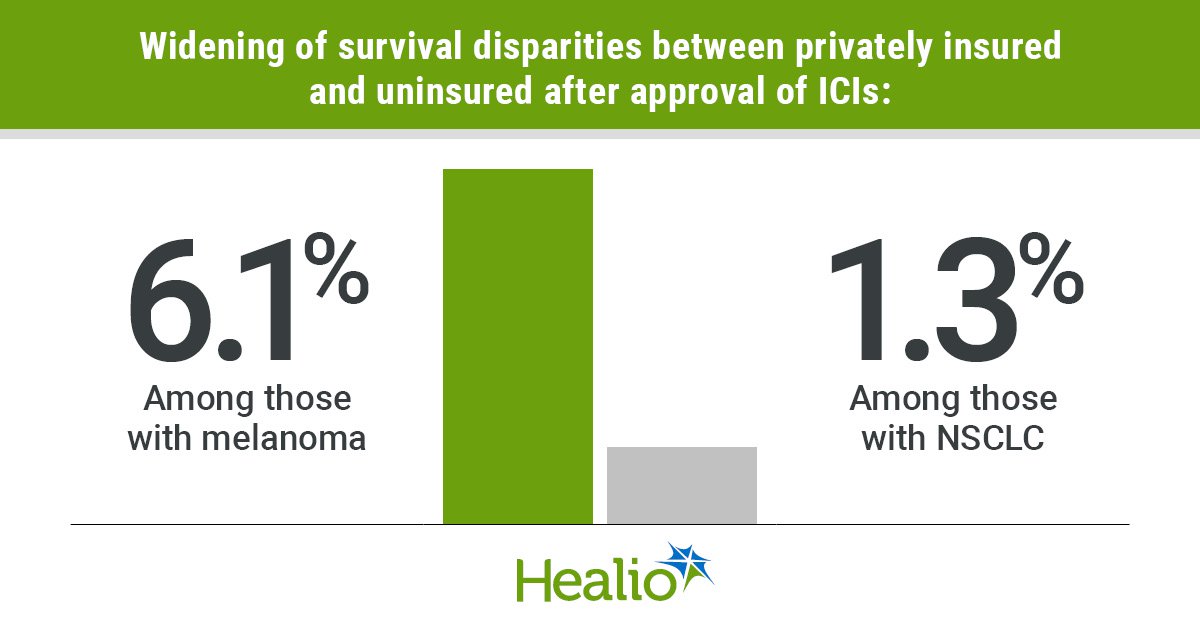
- Approval of immune checkpoint inhibitors has widened OS disparity for privately insured patients with melanoma or NSCLC vs. uninsured.
- Differences in private insurance vs. Medicaid have remained stagnant.
OS for stage IV melanoma, non-small cell lung cancer and renal cell carcinoma has substantially improved since the approval of immune checkpoint inhibitors, but insurance status has had a dramatic impact on who benefits most.
A cross-sectional analysis of more than 180,000 individuals showed a widening survival disparity between patients with private insurance and those who are uninsured.

Data derived from Zhao J, et al. JAMA Netw Open. 2025;doi:10.1001/jamanetworkopen.2025.19274.

Jingxuan Zhao
“Our findings underscore the importance of health insurance coverage, both private coverage and Medicaid coverage, in improving survival among adults younger than 65 years in the context of cancer treatment innovations,” Jingxuan Zhao, PhD, MPH, senior scientist of health services research at American Cancer Society, told Healio.
‘Long-standing disparities’
As of early 2025, the FDA had approved 11 immune checkpoint inhibitors (ICIs) for a combined 88 cancer indications, Healio previously reported.
ICIs have significantly improved OS for melanoma, NSCLC and renal cell carcinoma, among other malignancies.
Not everyone has access to these therapies though.
“In the U.S., having health insurance coverage is one of the strongest predictors of survival following a cancer diagnosis, and there are long-standing disparities in cancer outcomes by health insurance coverage and socioeconomic status,” Zhao said. “We had concerns that the introduction of effective high-cost advanced therapies like immune checkpoint inhibitors could widen these disparities. Although ICIs are associated with substantial improvement in survival, people with lower incomes or without health insurance coverage may be unable to afford them due to their high costs, potentially leading to even greater disparities.”
Zhao and colleagues used the National Cancer Database to investigate.
They included 12,048 individuals diagnosed with stage IV melanoma between 2002 and 2019, and 171,392 diagnosed with stage IV NSCLC or renal cell carcinoma between 2010 and 2019.
In all, the cohort consisted of 183,440 patients (mean age, 55.5 years; standard deviation, 7; 56.5% men; 77% white).
Most individuals had private insurance (65%) or Medicaid (24.1%). Uninsured patients made up 10.9% of the cohort.
OS rates based on health insurance type served as the primary endpoint.
‘Ensure equitable access’
Two-year OS rates improved after the approval of ICIs for all investigated cancers, regardless of insurance, except for uninsured individuals with renal cell carcinoma.
For melanoma, OS improved from 28.7% to 46% for patients with private insurance, from 14.1% to 29.6% for those with Medicaid, and from 16.2% to 28.3% for the uninsured.
These improvements resulted in a 6.1 percentage-point increase in survival disparity between private insurance and no insurance.
For NSCLC, the survival disparity between individuals with private insurance and no insurance increased 1.3 percentage points (95% CI, 0.2-2.3).
Researchers did not observe any difference in disparity between private insurance and Medicaid for either cancer type.
“Because eligibility for Medicaid is based on having low income, which can mean that people face barriers to timely access and continuity of care, we thought we might observe growing disparities between people with Medicaid and private insurance, as well,” Zhao said. “However, the survival differences between people with Medicaid and private insurance did not change significantly with the introduction of ICIs. This finding suggests that Medicaid coverage improves access to highly effective and high-cost cancer treatment such as ICIs.”
OS disparities did not change significantly for individuals with renal cell carcinoma.
However, disparities increased for all three cancer types after researchers excluded data from the first year after approval of ICIs to account for “lags in uptake,” they wrote.
Zhao and colleagues acknowledged study limitations, including lack of data on changes in insurance status.
“People without health insurance coverage did not experience the same improvements in survival that people with health insurance coverage experienced,” Zhao said. “Given the increasing use of ICIs for many cancers in both early and late stages of diagnosis and for first-line treatment, as well as subsequent lines of treatment, it is important to ensure equitable access to these therapies.”
‘Policy efforts are needed’
Financial assistance programs and patient navigation programs are a good place to start reducing disparities.
“However, even with these programs, patients may experience delays in ICI treatment initiation due to uncertainties during the application process and lack of provider awareness,” Zhao said. “Therefore, it is important for physicians and other members of cancer care teams help patients navigate these programs.”
Federal and state governments also can improve access to insurance. Zhao described Medicaid expansion and the Health Insurance Marketplace as “critically important coverage options for people who do not have health insurance coverage.”
“Previous studies have shown that Medicaid expansion and Marketplace are associated with increases in health insurance coverage and care affordability and better health outcomes,” she said. “Of note, our findings that the magnitude of improvement in survival after FDA approval of ICIs was similar among people with private health insurance and Medicaid coverage for multiple cancers suggest that expanding Medicaid to individuals without health insurance coverage may improve their access to ICI treatment.”
Zhao and colleagues plan to monitor changes in federal legislation and its impact on care.
They also want to examine other high-cost therapies and if the impact on survival changes based on insurance type.
Regarding ICIs, they want to investigate the issue based on usage, not just approvals, and if financial assistance programs have been effective.
“Ongoing monitoring and policy efforts are needed to prevent further widening of disparities and to ensure that all patients can benefit from advances in cancer care,” Zhao said.
For more information:
Jingxuan Zhao, MPH, can be reached at jingxuan.zhao@cancer.org.