The American Thoracic Society has just released a new guideline on CAP. It’s also been a while since I last updated the IBCC chapter on CAP (10/22), so I’m revising the chapter and incorporating the new guidelines. Here are some of my thoughts on the latest developments in severe CAP.
ATS and IDSA are… breaking up?
- ATS and IDSA collaborated on producing CAP guidelines. However, the IDSA refused to approve the final product (leaving the ATS to issue guidelines on its own).
- It’s unclear why the IDSA refused to approve the final guideline.
- The IDSA is expected to release its own CAP guideline soon.
- This is a nice reminder that guidelines are merely guidelines (which often disagree with one another).
exclusion of immunosuppressed patients in ATS guidelines
- Please bear in mind that ATS guidelines exclude immunosuppressed patients (which is broadly defined to include patients with cancer, advanced HIV, organ transplantation, chronic steroids, chemotherapy, disease-modifying antirheumatic drugs, and biological immunosuppressive medications).
- Immunosuppressed patients are commonly encountered in everyday practice. Excluding these patients promotes the mismanagement of their care. It would be ideal to include these patients in standard guidelines, so their management could be updated more frequently.
ultrasonography
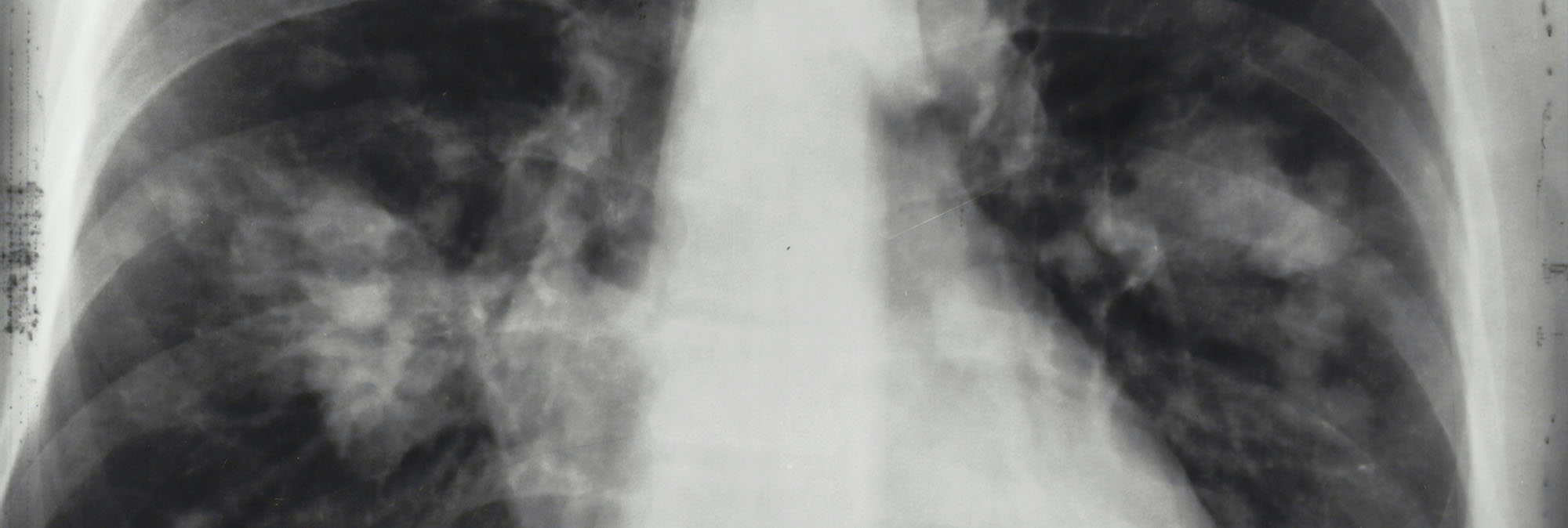
- The ATS guidelines “suggest lung ultrasound is an alternative diagnostic alternative to chest x-ray in medical centers where appropriate expertise exists (conditional recommendation, low-quality evidence). Vote: 13/15 committee members voted in favor of this recommendation.”
- Using POCUS instead of chest radiography is insane to me, and I don’t recommend this.
- Chest radiography and POCUS should be viewed as complementary studies, rather than competing modalities. The combination of POCUS plus chest radiography, together in the hands of an expert clinician, likely provides the best diagnostic utility.
- Chest radiography is a fundamental study used to track the progression of pneumonia over time and obtain a comprehensive surveillance view of the thorax. Neither of these is possible with lung ultrasonography.
- Research on lung ultrasonography is generally conducted with expert ultrasonographers, often in Europe, where everyone is skinny and wears skinny jeans. This may not translate well to other locations.
- In resource-limited settings without access to chest radiography, POCUS should be used accordingly.
- Studies on chest radiography, lung ultrasonography, and CT scans are hindered by the lack of a gold standard. A CT scan is often used as a gold standard in these studies, but it’s not truly a gold standard. In reality, CT scans often overcall pneumonia (which is a clinicoradiological diagnosis). If CT scans are used as a gold standard, this is frankly unfair to other imaging modalities (it will make chest radiography look less sensitive than it truly is).
inflammatory markers (CRP, procal)
- Disclaimer: These are not emergency medicine tests; they have zero role in the emergency department. If you’re an ED doctor who dislikes these tests, that’s fine; they’re not for you, so feel free to skip this section.
- Neither test should be used to determine whether to start antibiotics.
- Procalcitonin: can be helpful in questioning the diagnosis (particularly PNA versus aspiration pneumonitis or atelectasis). A low procalcitonin, supplemented with clinical judgment, can often help discontinue antibiotics quickly and redirect you to a correct diagnosis.
- CRP: Logistically, this is helpful to me because it comes back incredibly fast. CRP can help stratify the benefit from steroids if you’re on the fence about steroids (CRP >150 mg/L implies a lot of benefit from steroids; a normal CRP should question the pneumonia diagnosis altogether and cast doubt on the benefit from steroids). However, for a patient with a clear diagnosis of severe CAP, I wouldn’t delay starting hydrocortisone while waiting for CRP.
steroid for sCAP
- These are now recommended by ATS guidelines.
- Numerous meta-analyses support the benefit.
- I’ve discussed this before (e.g., here). Heck, I’ve been bullish on the use of steroids for severe CAP for >10 years (see this blog from 2015).
- Steroids should probably be given to most sCAP patients (but still exercise judgment about individual risks/benefits).
- I like hydrocortisone 50 mg IV q6hr because it was used in CAPE-COD and because it has very low CNS penetration (so it causes less delirium than agents like methylprednisolone). Also, hydrocortisone is relatively short-acting so if you decide to stop it, it’s easily shut off. (Deep dive on steroid pharmacology here).
- Steroids should be stopped when the patient is no longer critically ill due to their pneumonia (i.e., they could be transferred to the floor from a pneumonia perspective).
atypical coverage
- Needed in sCAP.
- My favorite drug for atypical coverage is doxycycline. Yes, I know that it’s often listed as second-line in many guidelines.
- Doxycycline is frankly more of a real antibiotic, whereas azithromycin primarily functions as an immunomodulator in 2025 (with rising levels of azithromycin-resistant Mycoplasma, azithromycin is starting to lose even atypical coverage). And now that we’re giving hydrocortisone to most patients, the need for azithromycin to dampen the immune system seems less important.
- The only real advantage of azithromycin is for Legionella (doxy probably works, but there’s more data for azithromycin).
- More details on the smackdown between doxy vs. azithromycin here.
beta-lactam backbone
- The 2023 ERS/ESICM/ESCMID/ALAT guidelines suggest the use of risk-stratification tools to determine whether broad-spectrum coverage is needed. (37012484) This seems like a better solution than using vibes.
- Remember that you’re not shooting for 100% coverage of any possible pathogen. A coverage rate of somewhere around ~90-95% might strike a reasonable balance between inadequate antibiotic coverage and excessively broad antibiotics.
- The DRIP score is emerging as a useful evidence-based tool to determine whether pseudomonal coverage is necessary.
- It is difficult to make any firm recommendations here, as this depends strongly on your local antibiogram and rates of MRSA and Pseudomonas.
duration of antibiotic therapy
- This is likely the most significant change in the new ATS guidelines.
- For patients with severe CAP who reach clinical stability and don’t have exclusion criteria, antibiotics can be stopped after 5 or 6 days of therapy.
- For patients with non-severe CAP, antibiotics can be stopped after 3-4 days. Pragmatically speaking, if a patient reaches clinical stability within 3-4 days, it’s likely that they had a mild CAP to begin with, so antibiotics can be stopped (a true severe CAP is quite unlikely to fully resolve within 3-4 days).
- In practice, patients can be clinically evaluated for antibiotic discontinuation between 3 and 6 days after initiation. After seven days, antibiotics should generally be stopped (as is already standard therapy).
- More details and exclusion criteria are discussed here.
That’s all for now. For more, see the full IBCC chapter on sCAP here. The chapter is reformatted into a top section that functions as a clinical checklist, and a bottom section that provides additional reference material for selective use.
Image credits: Photo by National Cancer Institute on Unsplash
Latest posts by Josh Farkas (see all)