[ad_1]
September 03, 2025
2 min read
Key takeaways:
- People with hidradenitis suppurativa have a greater risk for atherosclerotic cardiovascular disease, yet many are undertreated.
- Dermatologists should screen these patients for cardiometabolic risk factors.
Adults with severe hidradenitis suppurativa have more cardiometabolic risk markers, including high blood pressure and hyperlipidemia, putting them at greater lifetime risk for atherosclerotic cardiovascular disease, data show.
“Many patients with HS also have metabolic comorbidities, such as obesity or metabolic syndrome,” Michael S. Garshick, MD, a preventive cardiologist and director of the Cardio-Rheumatology Program at NYU Langone Health and assistant professor of medicine and dermatology at NYU Grossman School of Medicine, told Healio. “We wanted to understand the prevalence of some of these metabolic comorbidities in a large cohort of people with HS, as well as the relationship with HS disease severity. This is even more pertinent now because we are starting to explore how GLP-1 receptor agonists targeting metabolic dysregulation, whether it is obesity, metabolic syndrome or diabetes, can also modulate inflammatory conditions.”

Data derived from Dons M, et al. JAMA Dermatol. 2025;doi:10.1001/jamadermatol.2025.2989.
For the retrospective cross-sectional analysis, researchers analyzed data from 1,045 adults with HS who were identified from the NYU Langone Health database, assessing their 10-year and lifetime atherosclerotic cardiovascular disease (ASCVD) risk and cardiometabolic disease burden. The researchers categorized HS severity according to the treatment patients received: Mild (no medications or topicals only; 41.8%); moderate (oral therapies; 42%); or severe (biologics and/or surgery; 16.2%). Researchers defined ASCVD risk equivalents as established ASCVD, type 2 diabetes or a 10-year ASCVD risk score of 20% or greater.
The findings were published in a research letter in JAMA Dermatology.
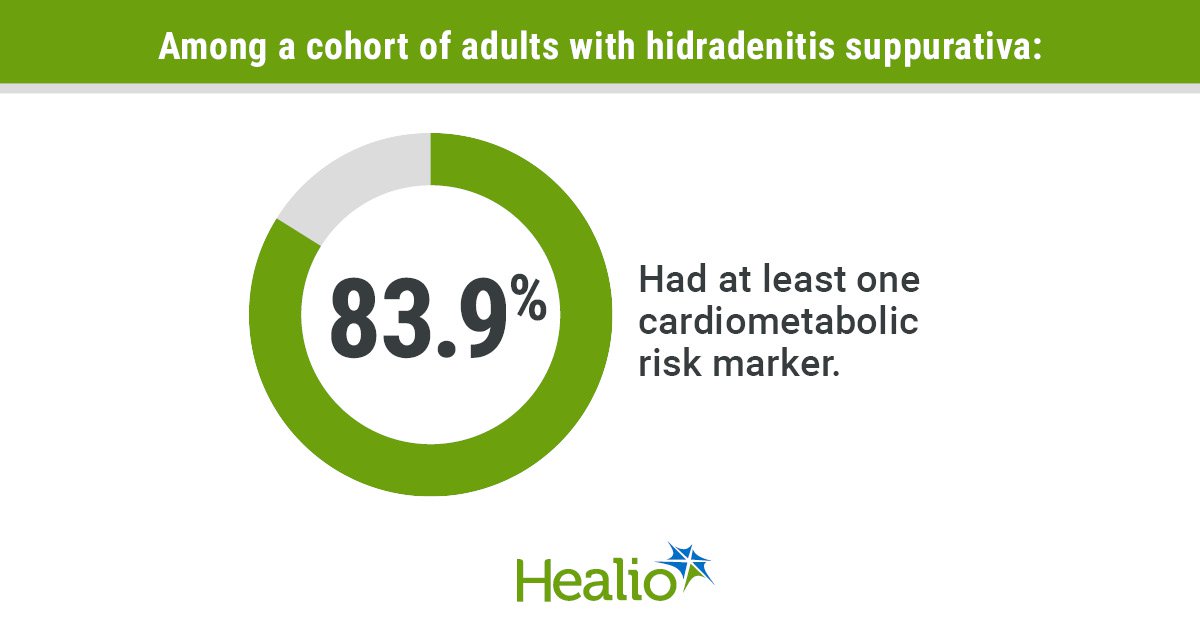
Nearly 40% of patients had either obesity (39.1%) or metabolic syndrome (36.1%) and most (83.9%) had at least one cardiometabolic risk factor.
Assessing individual risk markers for ASCVD, hyperlipidemia (34.3%), hypertension (30%) and diabetes (21.2%) were prevalent among patients; however, the researchers observed that severe HS was associated with a worse cardiometabolic profile compared with mild or moderate HS.
The mean lifetime ASCVD risk score was 16.18% for people with mild HS, 16.46% for those with moderate HS and 17.43% for those with severe HS (P = .03).
“What was interesting to us was the relationship between the degree of cardiometabolic risk factors and HS severity,” Garshick told Healio. “That goes along with some of these shared pathways between inflammatory conditions like HS and metabolic dysregulation, specifically obesity, which is highly proinflammatory. This overlap was not necessarily unexpected, but I do not believe it’s been shown that robustly before.”
Researchers also noted that although most patients with HS had an HbA1c of 7% or lower, only 55.1% of patients achieved blood pressure control targets and 47.5% achieved LDL cholesterol targets, yet just 22.8% of patients were prescribed antihypertensive therapies and 17.5% of patients were prescribed statins. These numbers were much lower for patients with HS and one or more ASCVD risk equivalent, Garshick said.
Garshick said it is important for clinicians to understand that even if patients see multiple health care professionals, screening for and treating cardiometabolic risk factors could still get overlooked — and it may fall to dermatologists to start the conversation.
“We must advocate for awareness that these patients with HS do have elevated cardiometabolic risk,” Garshick told Healio. “We need to get comfortable about counseling patients and saying, ‘We know that HS is associated with heightened cardiovascular and cardiometabolic risk. The more severe your HS disease, the more likely you are to have these risk factors. So, if you have not been screened for high blood pressure, hyperlipidemia, or diabetes, you should be screened. And, we have a lower threshold to treat you because we know that this risk exists.’ The ultimate goal is to have the dermatologist doing some of this [screening] themselves.”
For more information:
Michael S. Garshick, MD, can be reached at michael.garshick@nyulangone.org
[ad_2]
Source link