August 14, 2025
2 min read
Key takeaways:
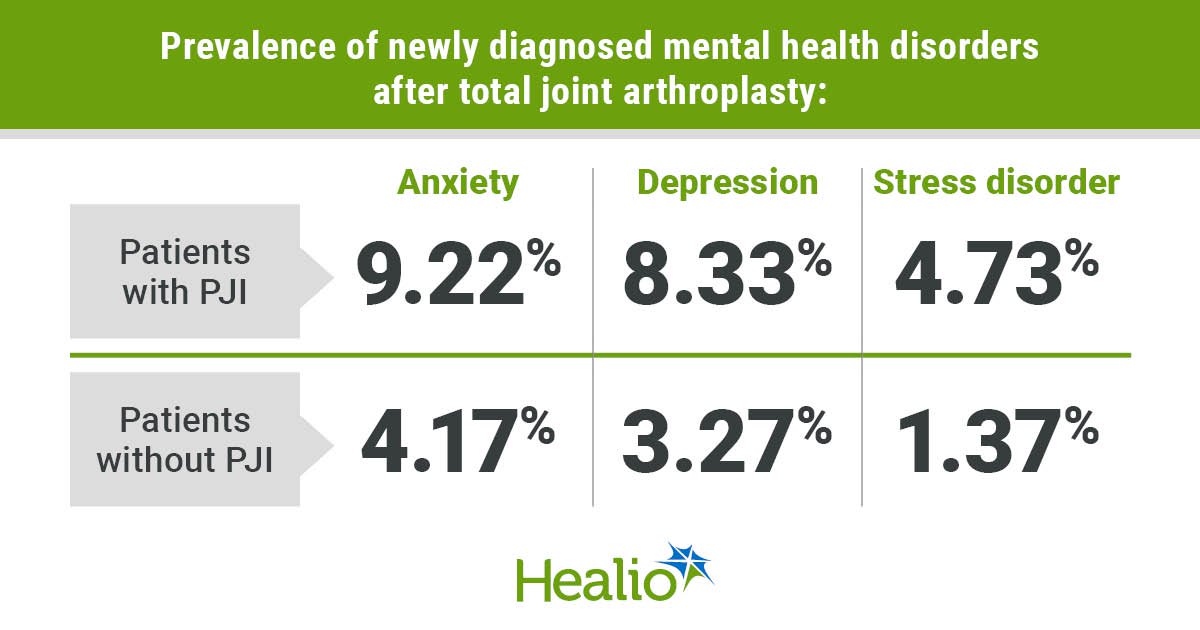
- Periprosthetic joint infection after joint arthroplasty led to a higher prevalence of new diagnosis of mental health disorder.
- Noninfection-related issues may also lead to new mental health disorders.
JERSEY CITY, N.J. — Patients who developed early periprosthetic joint infections after total joint arthroplasty had a higher prevalence of new diagnosis of mental health disorders, according to results presented here.
“These findings underscore the importance of early psychological support and screening for patients undergoing revision surgery and especially those who will undergo revision for periprosthetic joint infection,” Alvaro Ayala, MD, infectious disease fellow at Stanford University, Stanford Healthcare, told Healio.

Data were derived from Furukawa D, et al. Paper 1564. Presented at: Musculoskeletal Infection Society Annual Meeting; Aug. 1-2, 2025; Jersey City, N.J.
Ayala and colleagues retrospectively collected data for 25,608 patients who underwent total hip or knee arthroplasty from January 2015 to March 2025. Patients were categorized into groups based on whether they developed early PJI within 3 months of initial surgery, experienced mechanical or aseptic loosening within 3 months of initial surgery, or did not require revision.

Alvaro Ayala
“We collected demographic data, and we compared the incidence of mental health diagnosis within 1 year of total joint arthroplasty,” Ayala said in his presentation at the Musculoskeletal Infection Society Annual Meeting. “Then we performed our regression analysis, adjusting for age and gender.”
In his presentation, Ayala said 96% of patients did not have any complications, 3.14% were diagnosed with early PJI and 0.8% were diagnosed with noninfectious complications.
According to Ayala, patients who had PJI had a significantly higher prevalence of anxiety (9.22% vs. 4.17%), depression (8.33% vs. 3.27%) and stress disorder (4.73% vs. 1.37%) compared with patients who did not have PJI.
“When we adjusted this by gender, age and comorbidities, we found patients [with PJI] had higher risk for anxiety, depression and stress disorder,” Ayala told Healio. “We found an odds ratio of more than 2.5 at increased risk for these disorders compared with patients who did not have any complications.”
However, he said there was no statistically significant difference in rates of anxiety, depression and stress disorder between patients with PJI and those with noninfection-related issues.
“We argued that still having any sort of surgery after the first total knee or hip arthroplasty will predispose you to some, unfortunately, worse mental health outcomes, but if you have periprosthetic joint infections you will be at increased risk for poorer mental health outcomes,” Ayala said.
For more information:
Alvero Ayala, MD, wishes to be contacted through Lisa Kim at likim@stanfordhealthcare.org