September 08, 2025
4 min read
Inclusion cysts of the ocular adnexa are not uncommon. They often are asymptomatic and rarely present symptoms, depending on size and location.
Post-surgical conjunctival cysts are seen following ocular surgeries. The most common conjunctival cysts are implantation cysts and retention cysts. Trivial trauma and rarely allergy can also induce the formation of such cysts. They are often unilateral and transparent. In this column, we would like to present a case of post-vitrectomy inclusion cyst showing oncocytic differentiation.

Source: Dhivya Ashok Kumar, MD, FRCS, FICO, FAICO, Amar Agarwal, MS, FRCS, FRCOphth, Manisha Saravanabavan, MBBS, and Padmapreetha Narendiran, MS, FMRF
Case summary
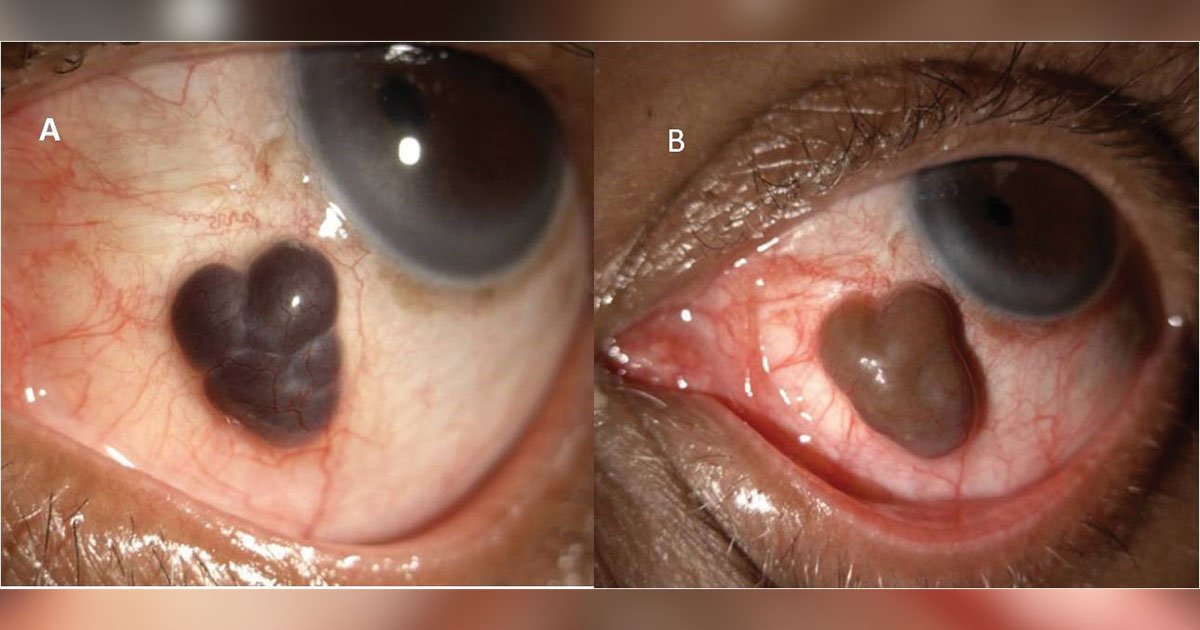
A 76-year-old man presented with complaints of a mass in the left eye for the past 6 months. His history included hypertension for the past 10 years. He had undergone a vitreoretinal procedure for bullous retinal detachment in the left eye a few months prior. The procedure was pars plana vitrectomy with silicone oil injection followed by silicone oil removal after 3 months. Best corrected visual acuity at presentation was 6/60, N24 in the left eye with an attached retina. On slit lamp examination, a pigmented mass about 4 mm × 5 mm with loculations was seen inferonasally surrounded by normal-appearing conjunctiva (Figure 1a). No tenderness or feeder vessels were noted.
Ultrasound biomicroscopy (UBM) showed an echoic lesion with no connection to the ocular coats or cavity (Figures 2a and 2b), confirmed by anterior segment OCT (Figure 2c). Because the lesion was asymptomatic, the patient was kept under observation. He was on regular follow-up, and by 6 months, there was a mild increase in the size of the lesion, and the color had changed to brownish-khaki (Figure 1b). MRI was performed to differentiate it from a uveal tumor, but no significant uveal changes were noted. After explaining the prognosis to the patient, he was advised to undergo mass excision biopsy with amniotic membrane graft with fibrin glue. This was performed under peribulbar anesthesia, and the excised mass was sent for histopathological confirmation.

The biopsy showed conjunctival mucosa composed of stratified squamous epithelium interspersed with goblet cells overlying a multilocular cystic lesion lined by multilayered large cells with eosinophilia granular cytoplasm and round to oval bland nuclei. The cells were suggestive of squamous cells, and the lumen of the cyst was empty, unlike a usual inclusion cyst of the conjunctiva. The probable histological diagnosis was that it could be a secondary conjunctival inclusion cyst with an oncocytic nature. The postoperative period was uneventful, and the conjunctiva healed without any recurrence (Figures 3a and 3b).

Conjunctival cyst
The symptoms of a conjunctival cyst depend upon its location. Traumatic cysts are usually seen in the region of the injury, and post-surgical cysts will be on the incision site. In cataract surgery, retention cysts occur comparatively more frequently with extracapsular cataract extraction than phacoemulsification. Also, they can appear following glaucoma filtering procedures and strabismus surgeries.

A Tenon’s cyst is formed by continuous epithelial serous secretion in a closed chamber after trauma to Tenon’s layer epithelial cells. Large cysts can occlude the punctum and induce epiphora. They can simulate a trabeculectomy bleb if they are noted at the 12 o’clock position. They can enlarge in size and cause discomfort on the superior cornea, and they are rarely visible in the palpebral aperture showing cosmetic disfigurement.
Post-vitrectomy cyst
Similar to post-cataract cyst formation, vitreoretinal procedures can also form secondary implantation cysts. Pars plana vitrectomy ports are often the source of the cysts. During silicone oil removal, the emulsified oil can exteriorize under Tenon’s capsule and tends to cause persistent inflammation, Moreover, the surgical tissue trauma to Tenon’s epithelium can also trigger cyst formation. Many times, the epithelium is exposed in an abnormal position and starts to secrete transudate.
Cyst mimics uveal prolapse or melanoma
In our case, there was heme that mimicked melanoma or uveal prolapse. The presence of heme created a pigmented appearance and challenged clinical differentiation. Use of anterior segment OCT and UBM can aid in such situations. As UBM was not confirmatory, we obtained an MRI to rule out a ciliary body tumor. The MRI did not show any mass lesion pertaining to the cyst location. By performing routine ultrasound B-scan, we were able to assess the posterior segment as well. Dilated fundus examination with indentation helps to evaluate the posterior segment changes beneath the conjunctional cyst. The pigmented appearance of the cyst in our patient was unusual and unlike a typical retention cyst, which is often transparent. Moreover, the loculated appearance perplexed us with the close differential diagnosis of a uveal tumor.
Conclusion
“Oncocytic lesions of the ocular adnexae are typically well-circumscribed cystic lesions that most often involve the caruncle,” Say and colleagues wrote in Ophthalmic Plastic and Reconstructive Surgery. “Epithelial cells with copious quantities of intensely eosinophilic cytoplasm characterize oncocytic transformation.”
Although these cysts are rare, they are not uncommon. Surgical removal is the line of management in such cases. Proper evaluation including clinical history, assessment, imaging and fundus examination can help confirm diagnosis and management.
- References:
- Narayanappa S, et al. Indian J Ophthalmol. 2010;doi:10.4103/0301-4738.67067.
- Nath K, et al. Indian J Ophthalmol. 1983:31(1):1-4.
- Sagoo MS, et al. Ophthalmic Plast Reconstr Surg. 2008;doi:10.1097/IOP.0b013e3181606835.
- Say EA, et al. Ophthalmic Plast Reconstr Surg. 2012;doi:10.1097/IOP.0b013e31822dd236.
- For more information:
- Amar Agarwal, MS, FRCS, FRCOphth, director of Dr. Agarwal’s Eye Hospital and Eye Research Centre, is the author of several books, including Phaco Nightmares: Conquering Cataract Catastrophes, Bimanual Phaco: Mastering the Phakonit/MICS Technique, Dry Eye: A Practical Guide to Ocular Surface Disorders and Stem Cell Surgery and Presbyopia: A Surgical Textbook. He can be reached at aehl19c@gmail.com; website: www.dragarwal.com.