Have you been diagnosed with a herniated disc or lumbar disc disease?
Are you looking for precise, reassuring information on their evolution, symptoms and treatments?
Answers from a physiotherapist!
♻️ Last update: Juny 30, 2025.
👩⚖️ Declaration of financial interests: none directly related to the subject. My complete declaration of financial interests is available in the legal notice section.
Written by Nelly Darbois, physiotherapist and scientific editor
What exactly is a herniated disc?
Your spinal column is made up of vertebrae, small bones stacked on top of each other to form your back. Between each vertebra there’s an intervertebral disc, like a soft cushion that absorbs shocks and allows movement.
Inside the spinal column is the spinal cord, which carries information between your brain and your body. On either side of the vertebrae, nerves exit the spinal column and travel to the arms, legs and other parts of the body.
When a disc becomes damaged (disc disease) or displaced (as in a herniated disc), it can press on a nerve.
Herniated disc
A herniated disc is when a disc between two vertebrae slips slightly out of place. It can press on a nerve and cause pain, tingling or loss of strength… but not always!
Some hernias go unnoticed and cause no symptoms.

Lumbar disc disease
Lumbar disc disease is different. It’s a progressive wear and tear of the disc, which can be linked to age or stress on the back. Again, this can lead to nerve compression.
Disc disease does not necessarily cause herniation, and herniation can exist without disc disease.

Lumbar, thoracic or cervical?
Both disc herniation and disc disease can occur at any level of the spine:
- Lumbar (lower back): this is the most common. It can cause pain in the lower back (lumbago) and/or sciatica (pain, tingling or weakness in one leg).
- Cervical (neck): can cause neck pain, headaches, and sometimes cervicobrachial neuralgia (pain and numbness in one arm).
- Thoracic (mid-back): rarer, it can cause pain in the back or around the thorax.
The good news is that many hernias are discovered by chance, without symptoms, and do not necessarily require surgery!
🔎 An analysis of 20 studies evaluated the results ofMRI scans carried out on people with no symptoms (no pain or discomfort). The results show that disc abnormalities are very common, even in people with no back pain:
- 2 to 8 out of 10 people had a drop in signal intensity, a sign of disc aging (discopathy)
- 1 to 8 out of 10 people had a bulging disc (slightly protruding disc; herniation)
- 0 to 6 out of 10 people had a disc protrusion (disc that protrudes a little further; herniation)
- 0 to 2 in 10 people showed disc extrusion (part of the disc that protrudes straight out; herniation)
- 0 to 6 out of 10 people had a narrowing of the disc(disc disease)
- 0 to 6 in 10 had annular fissures (small tears in the disc wall; disc disease)
Source : Donnally 2023
👉 What this means: many people have disc abnormalities visible on MRI without experiencing pain. So finding a herniated or damaged disc on MRI doesn’t necessarily mean it’s the cause of the pain. In the absence of pain or discomfort in movement, specialized medical advice is often not necessary.
What are the symptoms of a herniated disc?
It all depends on location and “severity”! Sometimes, you may have a herniated disc… without even knowing it (it’s discovered by chance, and there’s no need to do anything special!).
But when it presses on a nerve, it can give :
- Local pain: in the lower back (lumbar hernia) or neck (cervical hernia).
- Radiated pain: sciatica (leg) or cervicobrachial neuralgia (arm).
- Numbness, tingling in a limb.
- Loss of strength in the leg or arm (rarer).
What is the recovery time for herniated discs and lumbar disc disease?
Here are some typical timescales for the evolution of a herniated disc that causes pain.
- Acute pain: often 3 to 6 weeks for clear improvement.
- Resorption of the hernia (it sometimes disappears): around 3 to 12 months, but without necessarily any troublesome symptoms during this time.
- Cases requiring more time: if pain is intense or nerves are affected, recovery may take longer.
📌 The most important thing? 🏃♂️ Move (without forcing) and adapt your activities.
Unlike a herniated disc, lumbar disc disease doesn’t really “heal”… but that doesn’t mean the pain is permanent! 😊
- Painful phase: may last from a few weeks to a few months, depending on inflammation.
- Adaptation of the body: over time, the back finds other strategies for pain-free movement.
- Evolution: discopathy is a progressive wear and tear of the disc, but you can live with it without daily discomfort!
How long should I stop working because of a herniated disc or lumbar disc disease?
Work stoppage is not systematic for these pathologies.
This depends on several factors:
- pain intensity,
- the type of work,
- and the evolution of symptoms.
Herniated discs: downtime can range from a few days to several weeks, especially if the pain is severe or there is sciatica. Most people resume in 2 to 6 weeks.
Lumbar disc disease: often, there’s no need for prolonged downtime. Just adapt the workstation or take regular breaks to avoid aggravating the pain.
📌 Good to know: total rest is not recommended for too long. Resuming a suitable activity helps recovery! 🚶♂️💼
What treatments are recommended?
In most cases, a herniated disc gets better on its own ! 🎉
We treat only if symptoms (pain, loss of strength) are too troublesome.
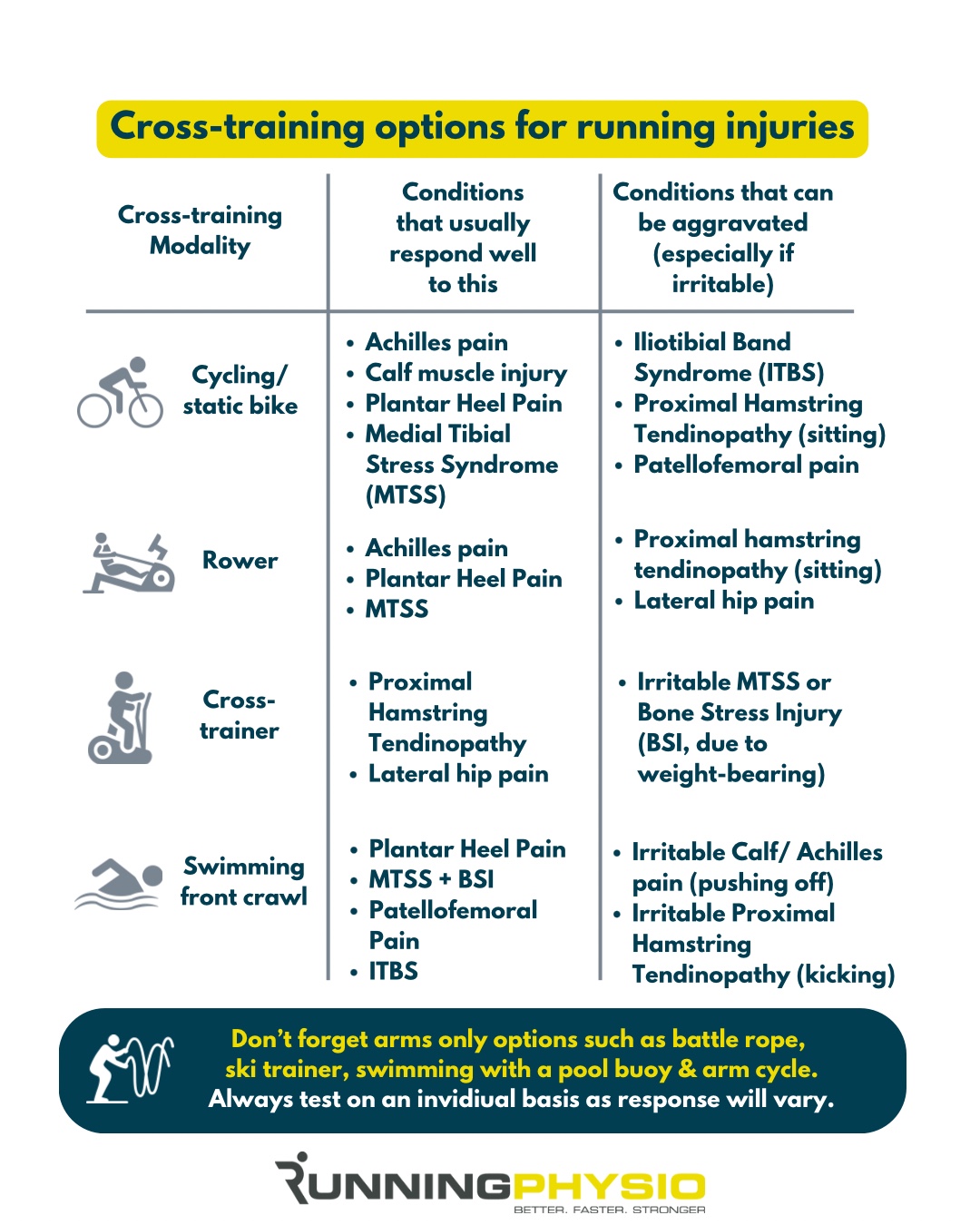
Exercise and physiotherapy
Adapted physical activity helps prevent stiffening.
Progressive movement is essential to prevent chronic pain: the less you move, the more painful the movement may be, even though it doesn’t aggravate the hernia.
If prescribed, physiotherapy often includes :
- targeted muscle-strengthening exercises (sheathing, deep back and abdominal muscle work). It is thought that working the postural muscles, in particular the transversus abdominis and paravertebral muscles, can compensate for the loss of disc support (in cases of disc disease);
- gentle stretching. Spinal mobility and flexibility exercises are thought to help maintain good muscle balance and reduce pressure on spinal joints.
- support to help you identify the right amount of physical activity for you, and the type of activity: neither too much nor too little;
- sometimes manual therapy, massage or the application of TENS.
🔎 A research team has synthesized studies on the effect of sport and loads on intervertebral discs.
📌 What they found:
- Good for the discs 🏃♂️: dynamic efforts, in the axis of the spine, at moderate speed, and of similar intensity to walking or jogging seem beneficial.
- Bad for disks ⚠️ :
- Static loads (staying in one position for a long time)
- Twisting the back under load
- Compression flexion (bending forward with weight)
- Rapid movements or intense shocks (explosive exercises, strong impacts)
📉 Not moving is also bad: lack of activity weakens the discs.
The study also mentions that genetics play a role, and that there may be a “critical period” in disc development when exercise has a lasting impact.
Source: Belavy 2016
Medicines
Drug treatments include :
- analgesics(paracetamol, non-steroidalanti-inflammatory drugs in the absence of contraindication),
- and, in some cases, muscle relaxants to reduce secondary muscle contractures.
Operation?
Surgery is exceptional, and reserved for cases where pain persists despite several months of conservative treatment, or when severe neurological damage appears (severe muscle weakness, loss of sensitivity, cauda equina syndrome).
Infiltration may be tried before considering a more invasive solution.
For herniated discs, the most common procedure is a discectomy, which removes the part of the disc compressing the nerve.
Arthrodesis, which consists in fixing two vertebrae together to stabilize the spine, can be proposed in severe forms where the disc no longer plays its role as a shock absorber.
🔎 One of the most cited studies on the results of surgery compared with non-surgical treatments for lumbar disc disease is the SPORT (Spine Patient Outcomes Research Trial). Its findings show that patients who chose surgery had better outcomes at 3 months, 2 years and 4 years compared with those who opted for conservative treatment.
However, the choice of surgical technique remains a subject of study. Microdiscectomy and conventional open surgery offer broadly similar results. A “limited” discectomy provides better pain relief and improves patient satisfaction, but is associated with a higher risk of recurrence than a larger discectomy. In the event of recurrence, a second microdiscectomy gives comparable results to the first procedure.
Surgery is often performed on an outpatient basis, but in some cases an overnight hospital stay may be necessary. It’s important to note that while surgery is effective in relieving sciatic pain (radiating down the leg), its results are less predictable for non-irradiated lumbar pain.
Source : Donnally 2023
***
That’s all I wanted to say on the subject! Any questions or comments? See you in comments!
You may also be interested in these articles
📚 SOURCES
Donnally III CJ, Hanna A, Varacallo MA. Lumbar Degenerative Disk Disease. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134/
Belavý DL, Albracht K, Bruggemann GP, Vergroesen PP, van Dieën JH. Can Exercise Positively Influence the Intervertebral Disc? Sports Med. 2016 Apr;46(4):473-85. doi: 10.1007/s40279-015-0444-2. PMID: 26666742.
Belavý DL, Albracht K, Bruggemann GP, Vergroesen PP, van Dieën JH. Can Exercise Positively Influence the Intervertebral Disc? Sports Med. 2016 Apr;46(4):473-85. doi: 10.1007/s40279-015-0444-2. PMID: 26666742.