This compelling study challenges long-held assumptions about the diagnosis of early systemic sclerosis.
Many of us rely on the presence of puffy hands — or, by the time patients are seen, sclerodactyly, Raynaud’s phenomenon (RP) and a positive ANA — to make the diagnosis. Since 95% of patients with SSc have both RP and a positive ANA, the absence of either typically leads us to consider alternative diagnoses, such as scleroderma mimics or early rheumatoid arthritis.
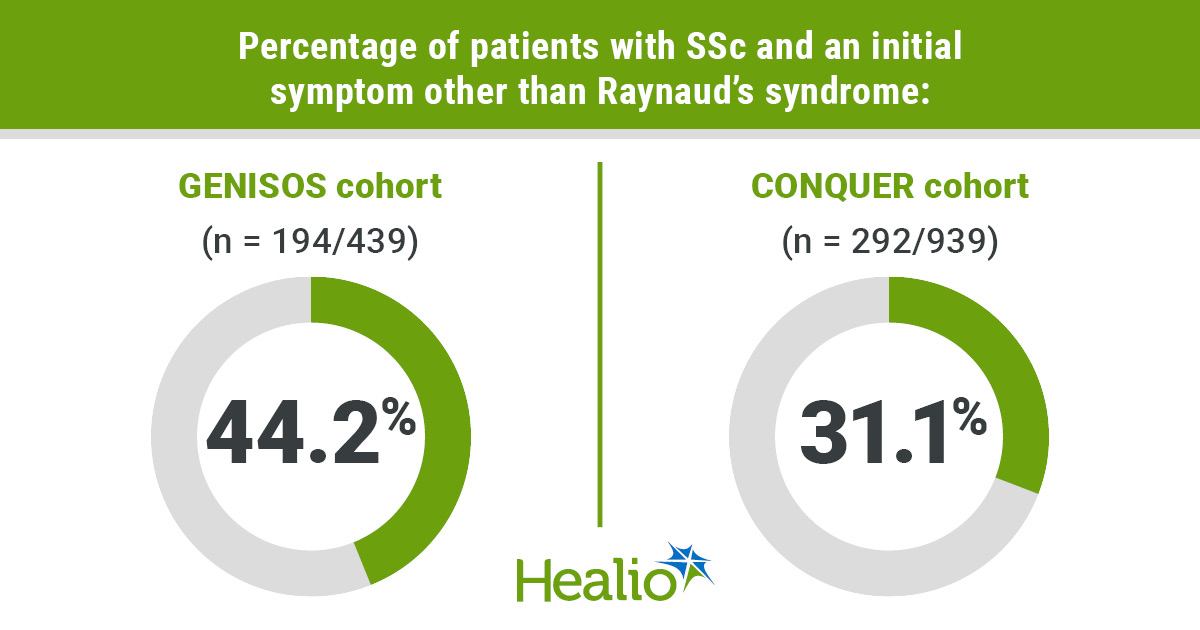
Traditionally, SSc without RP or ANA has been considered rare and diagnosed cautiously. However, this study found that more than 30% of patients with early SSc had symptoms other than RP as their first clinical manifestation. These “non-RP-first” patients were more likely to have diffuse cutaneous disease and joint contractures at enrollment. They also had a higher prevalence of anti-RNA Polymerase III antibodies (26% vs. 14% in RP-first patients).
Meanwhile, 95% of patients tested positive for ANA using HEp-2 IFA, with speckled being the most common staining pattern. Nucleolar, centromere and homogenous patterns were also observed. Importantly, only about 50% of patients screened using multiplex ANA panels tested positive, vs. more than 90% with HEp-2 IFA. This highlights a key limitation of multiplex assays, which often miss RNA Polymerase III and other SSc-specific autoantibodies.
The findings underscore two major pitfalls in early SSc diagnosis — assuming RP must be the first symptom and relying on less sensitive multiplex ANA panels. This paper is an important reminder to maintain a high index of suspicion and to use appropriate serologic testing when evaluating patients for early SSc.
David A. McLain, MD, MACR, FACP, FRCP
Executive director
Alabama Society for the Rheumatic Diseases
Symposium director
Congress of Clinical Rheumatology
Disclosures: McLain reports no relevant financial disclosures.