October 08, 2025
3 min read
Key takeaways:
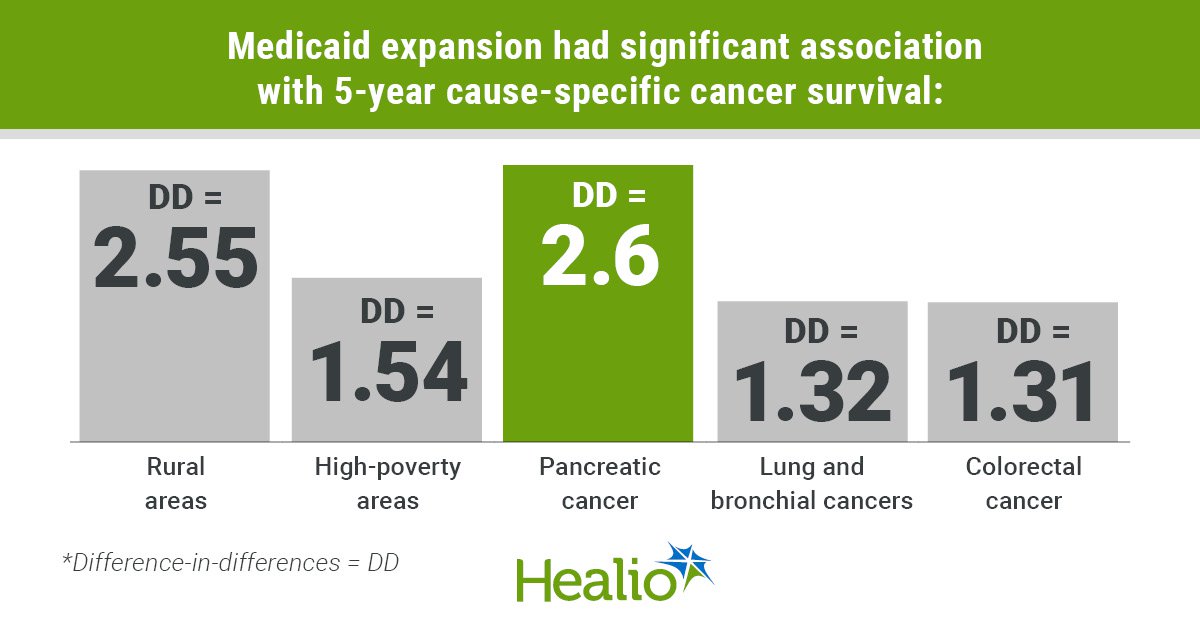
- Medicaid expansion significantly improved 5-year survival for individuals with cancer living in rural areas and impoverished communities.
- Patients with lung, pancreatic and colorectal cancers also benefited.
Medicaid expansion has significantly improved long-term survival outcomes for patients with cancer who live in rural communities and high-poverty areas.
Expanding coverage also has improved survival from malignancies with high mortality, including colorectal, lung and bronchial, and pancreatic cancers.

Data derived from Schafer EJ, et al. Cancer Discov. 2025;doi:10.1158/2159-8290.CD-25-1244.

Elizabeth J. Schafer
“The evidence supporting Medicaid expansion in improving outcomes for cancer patients is clear,” Elizabeth J. Schafer, MPH, associate scientist in surveillance, prevention and health services research at American Cancer Society, told Healio.
“Research has shown that Medicaid expansion can increase cancer screening prevalence, early-stage diagnosis, short-term survival and now 5-year survival. These findings highlight the need to advocate for the protection of Medicaid expansion to avoid jeopardizing progress in reducing the cancer burden.”
Medicaid expansion
The Patient Protection and Affordable Care Act, which went into effect in 2014, allowed states to expand Medicaid coverage to adults with incomes up to 138% of the federal poverty level.
As of June 2025, 40 states and the District of Columbia had expanded Medicaid coverage, with Oklahoma, Missouri, South Dakota and North Carolina joining the list between 2021 and 2023, according to healthinsurance.org.
States that have not expanded eligibility yet include Alabama, Georgia, Florida, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin and Wyoming.
Prior studies have shown that expansion lowers uninsurance rates, increases both cancer screening and early-stage diagnoses, and improves 2-year OS among individuals with a new cancer, according to study background.
Schafer described research into the long-term impacts of Medicaid expansion as “crucial.”
Researchers used the Cancer in North America Survival dataset to compare survival rates before and after expansion.
They evaluated 1,423,983 adults aged 18 to 59 years (55.3% women; 71.7% white) diagnosed with cancer between 2007 and 2008 and 2014 and 2015. They included patients who lived in 26 states that expanded Medicaid coverage in 2014 and in 12 states that had not as of 2020.
Cause-specific 5-year cancer survival served as the primary endpoint.
‘Encouraging’ results
The cohort included 813,684 adults who were diagnosed with cancer in states that expanded Medicaid coverage and 610,299 diagnosed in states that did not.
States that expanded Medicaid had a higher rate of diagnosis of Black adults (17.9% vs. 9.1%) and those who lived in high-poverty areas (7.7% vs. 4.4%).
Cause-specific 5-year cancer survival increased at similar rates for expansion states (77.7% vs. 79.5%) and non-expansion states (75.1% vs. 77%).
However, researchers did find a significant association with expansion and cause-specific 5-year survival for patients who lived in rural areas (difference-in-differences [DD] = 2.55 percentage points; 95% CI, 0.23-4.86), those who lived in the highest county-level poverty areas (DD = 1.54; 95% CI, 0.3-2.77), white individuals (DD = 0.37; 95% CI, 0.05-0.7), and those with pancreatic cancer (DD = 2.6; 95% CI, 0.86-4.34), lung and bronchial cancer (DD = 1.32; 95% CI, 0.3-2.34), and colorectal cancer (DD = 1.31; 95% CI, 0.26-2.37).
Schafer and colleagues also observed a significant association with expansion and 5-year OS for patients who lived in rural communities (DD = 3.03 percentage points; 95% CI, 0.66-5.41), those who lived in high-poverty areas (DD = 1.69; 95% CI, 0.43-2.95), Black (DD = 1.05; 95% CI, 0.17-1.93) and white individuals (DD = 0.57; 95% CI, 0.24-0.91), and those with pancreatic (DD = 2.14; 95% CI, 0.52-3.76), lung and bronchial (DD = 1.58; 95% CI, 0.64-2.52), and colorectal cancer (DD = 1.2; 95% CI, 0.13-2.27).
“It is encouraging to see improvements in survival among patients residing in rural and high-poverty areas and among those patients diagnosed with more fatal cancers,” Schafer said. “Of note, individuals residing in these communities often experience significant disparities in insurance coverage and access to timely diagnostic and treatment services.”
Researchers acknowledged study limitations, including lead-time bias, which could have occurred with expanded screening and prevention opportunities under the Affordable Care Act.
Schafer emphasized the importance of future research into how work requirements for Medicaid, which go into effect in 2027 around the country, could impact uninsurance rates as well as cancer outcomes.
“This study was crucial for understanding the long-term effects of Medicaid expansion on survival outcomes among individuals diagnosed with cancer,” Schafer said. “The findings provide essential evidence to support informed decision-making by policymakers and advocates working to protect and further expand Medicaid coverage.”
For more information:
Elizabeth J. Schafer, MPH, can be reached at elizabeth.schafer@cancer.org.