[ad_1]
November 26, 2025
4 min read
Key takeaways:
- Patients with Medicaid coverage had significantly higher odds of experiencing interruptions in radiation therapy.
- Cancer type, marital status and radiation dose also had significant links to delays.
Treatment interruptions have been a long-standing issue with radiation therapy.
Researchers at University of Tennessee found nearly 25% of their patients missed at least two sessions between 2020 and 2024. Several factors were associated with delays, including malignancy type, marital status and insurance coverage, with patients on Medicaid having a significantly higher risk for both moderate and severe interruptions.

Data derived from Kumsa FA, et al. JCO Clin Cancer Inform. 2025;doi:10.1200/CCI-25-00218.
“The worst treatment for cancer is the treatment that’s never received,” David L. Schwartz, MD, FACR, professor and chair of the department of radiation oncology at The University of Tennessee Health Science Center, told Healio. “Understanding reasons why people don’t get to their treatment is absolutely crucial.”
‘It’s that important’
More than half of all individuals diagnosed with cancer receive radiation therapy, according to study background.
However, many patients do not get all their treatments, often due to toxicities and logistical issues like transportation.
“There have been publications dating back to the 1980s where you would see almost half of patients having considerable delays during a course of treatment,” Schwartz said. “When I came to Tennessee, I immediately saw a tremendous number of patients having considerable interruptions during their treatment. Even before COVID, we were documenting interruption rates approaching 30% for certain folks from at-risk populations.”
Prior research has shown treatment failure occurs more often among those who do not stick to their schedule.
“Not showing up for radiation treatment leads to survival differences similar to what is seen with successful phase 3 registration trials that the FDA uses to approve new cancer drugs. It’s that important. When you’re talking about more than 30% of patients not making it in for timely radiotherapy, you’re talking about therapeutically relevant outcome differences.”
Schwartz and colleagues used a large language model to evaluate risk factors associated with radiation treatment interruptions.
They evaluated behavioral, clinical, demographic and neighborhood-level data from 2,130 patients (50.8% aged 66 years and older; 93.7% white; 53.3% women) diagnosed with cancer who received radiation therapy at University of Tennessee Medical Center between August 2020 and May 2024.
Researchers grouped patients into three categories: no missed days (0-1 missed session), moderate delays (2-4) and severe interruptions (5 or more).
Number of missed radiation therapy days served as the primary endpoint.
Factors associated with delays
Overall, 15.7% of patients had moderate treatment interruptions and 7.7% had severe delays.
Moderate interruptions had a significantly greater chance of occurring among patients with genitourinary (adjusted OR = 3.81; 95% CI, 1.24-11.66) and prostate cancer (aOR = 2.44; 95% CI, 1.34-4.46) compared with breast cancer.
Patients with Medicaid coverage had a significantly higher likelihood of moderate delays than those with private insurance (aOR = 2.22; 95% CI, 1.32-3.73).
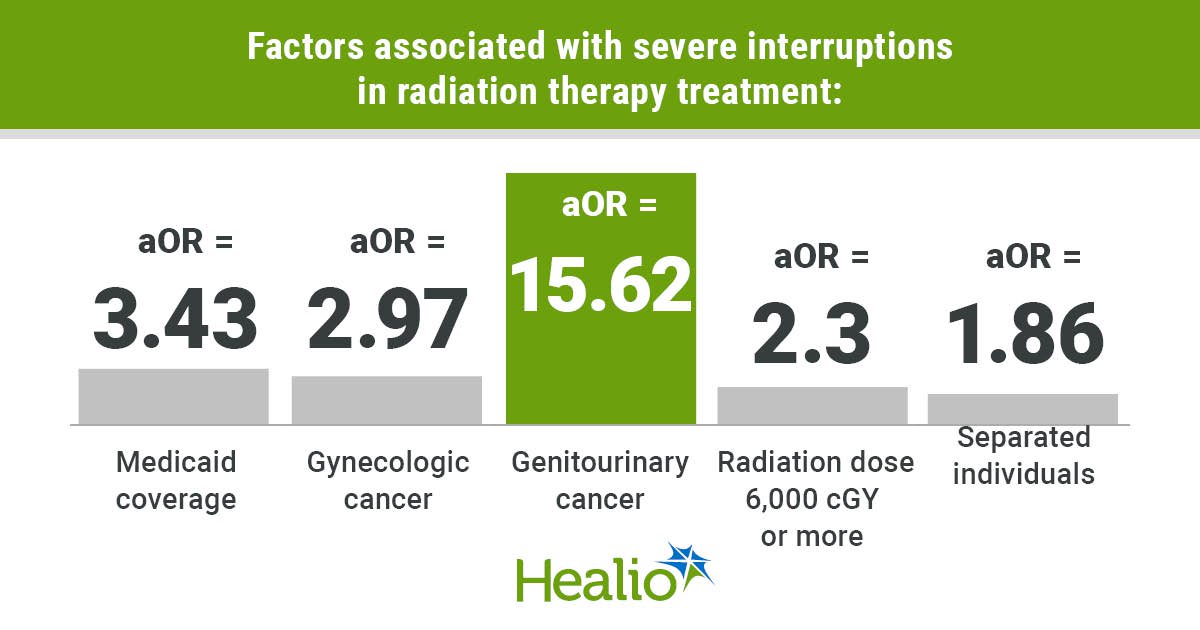
Medicaid coverage had a significant association with severe interruptions (aOR = 3.43; 95% CI, 1.77-6.64), too.
“Financial and process-related treatment access issues were the dominant predictors for treatment interruption, the most important being insurance coverage,” Schwartz said.
Severe delays also occurred more frequently among adults who were separated compared with married individuals (aOR = 1.86; 95% CI, 1.18-2.94), and among patients who lived in neighborhoods with a high Social Vulnerability Index (aOR = 2.6; 95% CI, 1.32-5.09).
Compared with breast cancer, severe interruptions had a significant association with gynecologic (aOR = 2.97; 95% CI, 1.3-6.79), head and neck (aOR = 2.31; 95% CI, 1.1-4.87) and genitourinary cancers (aOR = 15.62; 95% CI, 4.94-49.45). Race and ethnicity were not significant risk factors.
Severe interruptions also had a significant association with the length and dose of prescribed treatment, with delays more likely to take place during protracted courses of at least 6,000 cGy (aOR = 2.3; 95% CI, 1.09-4.88).
Researchers acknowledged study limitations, including lack of geographic and racial diversity, as well as its retrospective design.
‘Everybody needs a helping hand’
Schwartz and colleagues are currently conducting a prospective clinical trial funded by the Tennessee Department of Health evaluating radiation interruptions and patient-reported social risk factors. They have already found that many of the associations identified in this manuscript reappear as consistent themes.
“Access to information about cancer treatment was one of the most predictive factors for whether patients were able to get in for radiation treatment,” Schwartz said. “I’m not surprised, but to see it so plainly described by the patients themselves means that we are lapsing. We are not communicating well enough to find out what patients need.”
The researchers are currently performing formal qualitative studies with patients to hear why they are not coming in for treatment.
Common responses include lack of transportation, fear of treatment, patients preferring to “stay in bed,” “overwhelmed” caregivers, and toxicities, Schwartz said.
“Every patient with cancer, regardless of privilege, faces a unique and potentially daunting collection of social barriers to care,” Schwartz said. “Everybody needs a helping hand during cancer treatment, and we need to figure out ways to help everybody.”
The University of Tennessee Health Science Center has already implemented interventions to help address treatment lapses. A new grant-funded pilot trial supervised by Dr. Schwartz is centered on helping distressed patients presenting with newly found cancer through the emergency room. The group is taking advantage of digital health technology data to triage patients and connect them with personalized social support.
“It leverages the expertise of our Community Health Support Specialist Team who partner and lead with us through the UTHSC Office of Community Health Engagement,” Schwartz said. “It’s radically individualized support. It’s supercharged patient guidance that goes past what we typically define as navigation. Our specialists are now going to get hooked up by phone with patients just after their emergency room discharge to make sure they make it to their cancer treatment.”
Radiation oncologists can play a role, too, by abbreviating radiation courses via hypofractionation when possible.
“The single most important question is, ‘Are we making a clinically meaningful difference for patients to get to their treatment?’” Schwartz said. “And No. 2, can we do this in a financially sustainable way that payers will accept as necessary for coverage? We are doing the prospective studies to do that.”
Schwartz emphasized the role of AI-based informatics in this project. Led by the UTHSC-ORNL Center for Biomedical Informatics, the group uses novel explainable AI to capture individual patient social needs to guide intervention and educational support,
“Patients and providers alike are overwhelmed by the intense realities of modern oncology,” Schwartz said. “What we’re trying to do is to leverage today’s AI-driven user-centric technologies to overcome what are very stubborn, uniquely human problems.”
For more information:
David L. Schwartz, MD, FACR, can be reached at dschwar4@uthsc.edu.
[ad_2]
Source link