August 05, 2025
3 min read
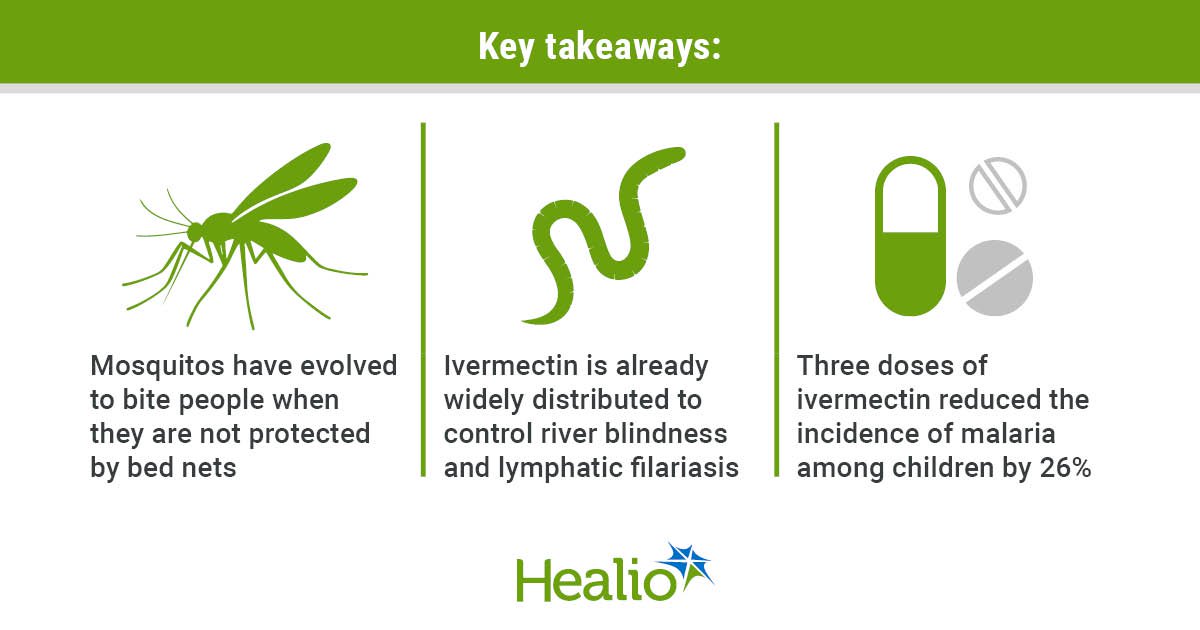
Key takeaways:
- Bed nets and insecticide spraying have reduced malaria, but progress has stalled, researchers said.
- Mass ivermectin dosing could help control malaria and other parasitic infections.
Mass administration of ivermectin reduced the incidence of malaria by 26% among children during a trial in Kenya, indicating that it could serve as another tool to prevent transmission in highly affected areas, according to researchers.
Bed nets treated with insecticide have been a “great success” for preventing malaria deaths, Carlos J. Chaccour, MD, PhD, a researcher at the Navarra Center for International Development at the University of Navarra in Pamplona, Spain, told Healio. From 2000 to 2015, malaria cases declined 81% in Africa thanks to treated bed nets and indoor residual spraying, Chaccour and colleagues wrote in The New England Journal of Medicine.

Derived from Chaccour C, et al. New Engl J Med. 2025;doi:10.1056/NEJMoa2411262.
“But remember Jurassic Park? Chaccour said. “‘Life finds a way.’”
Mosquitos have evolved to bite outdoors at dusk and dawn, when people are not protected by bed nets, which allows malaria to continue to spread, Chaccour explained. Additionally, he noted that malaria vaccines provide only partial protection, so a combination of multiple tools is needed to prevent transmission and eventually eliminate the disease.
Chaccour and colleagues evaluated whether mass distribution of ivermectin could be a tool for reducing malaria in communities where there is residual transmission. They conducted a cluster-randomized trial in Kwale, the county with the highest malaria burden in coastal Kenya.
“In Kwale, where our study took place, 85% of households own bed nets and 77% use [them] consistently, and yet we found that one in three kids had malaria parasites in them at baseline,” Chaccour said.
The researchers administered monthly doses of ivermectin or another antiparasitic drug not suitable for malaria control, albendazole, to 84 clusters comprising 28,932 people from October through December 2023. Half of the clusters received three doses of ivermectin (400 µg/kg), and the other half received albendazole (400 mg) as a control. Each cluster included 35 children aged 5 to 15 years, whom the researchers followed for 6 months after the first dose was administered to determine the efficacy of the treatment.
After 6 months, the researchers reported that ivermectin reduced the incidence of malaria in children by 26% compared with the control (2.2 per child-year vs. 2.66 per child-year; incidence rate ratio [IRR] = 0.74; 95% CI, 0.58-0.95).
Participants experienced 17 serious adverse events: nine deaths, seven hospitalizations and one medically relevant event, but none were drug related. Chaccour and colleagues did not find a significant difference in the prevalence of serious adverse events between the two groups. They also did not notice any safety concerns among the 103 pregnant women who received either medication.
Resistance has been a concern in these types of trials in the past, but Chaccour noted that Merck has donated up to 400 million ivermectin treatments every year for more than 30 years to control river blindness and lymphatic filariasis. After roughly 5.9 billion treatments have been administered, he said no signs of resistance were found. If the treatments begin being distributed on a larger scale, experts will need to monitor resistance among mosquitoes, he added.
“The fact that it is not to be used alone but in combination with bed nets and other antimalarial tools should help delay — if not prevent — the emergence of resistance,” he said.
Chaccour said his team intends to conduct a second study to share with WHO to inform possible policy updates. Future studies will evaluate four or five rounds of ivermectin, he said, and they may test a higher dose and livestock administration, as well.
“Because ivermectin is a broad-spectrum antiparasitic, it also reduces scabies, head lice, intestinal worms and filariae in the community,” Chaccour said. “These diseases are often coendemic because they are common in poor settings and rural areas. This provides endemic countries with an opportunity for an integrative approach, tackling five, six, seven diseases at once with a single pill in a single program. That is the breakthrough.”
References:
For more information:
Carlos J. Chaccour, MD, PhD, can be reached at cchaccour@unav.es.