September 26, 2025
2 min read
Key takeaways:
- Women, and especially women of color, remain underrepresented in clinical trials.
- This drives disparities in care, reinforces bias and creates outcomes that harm women and women of color across health systems.
CHICAGO — Although the U.S. population has become more diverse over the past decade, women, and especially women of color, remain underrepresented in clinical research, according to a speaker here.
“Our public health systems, our research agendas and our policy strategies, they have to evolve,” Heather M. Prendergast, MD, MS, MPH, MHA, FACEP, professor of emergency medicine and associate dean of clinical affairs at University of Illinois College of Medicine, said at the Power of Women in Medicine Summit. “Representation in research and in data is no longer optional. It is essential if we really want to address the system and secure the future of equitable care, public health and scientific discovery.”

Data were derived from Prendergast H. Invisible data, visible harm: Addressing the research gaps in women’s health for women of color. Presented at: Power of Women in Medicine Summit; Sept. 18-20, 2025; Chicago.
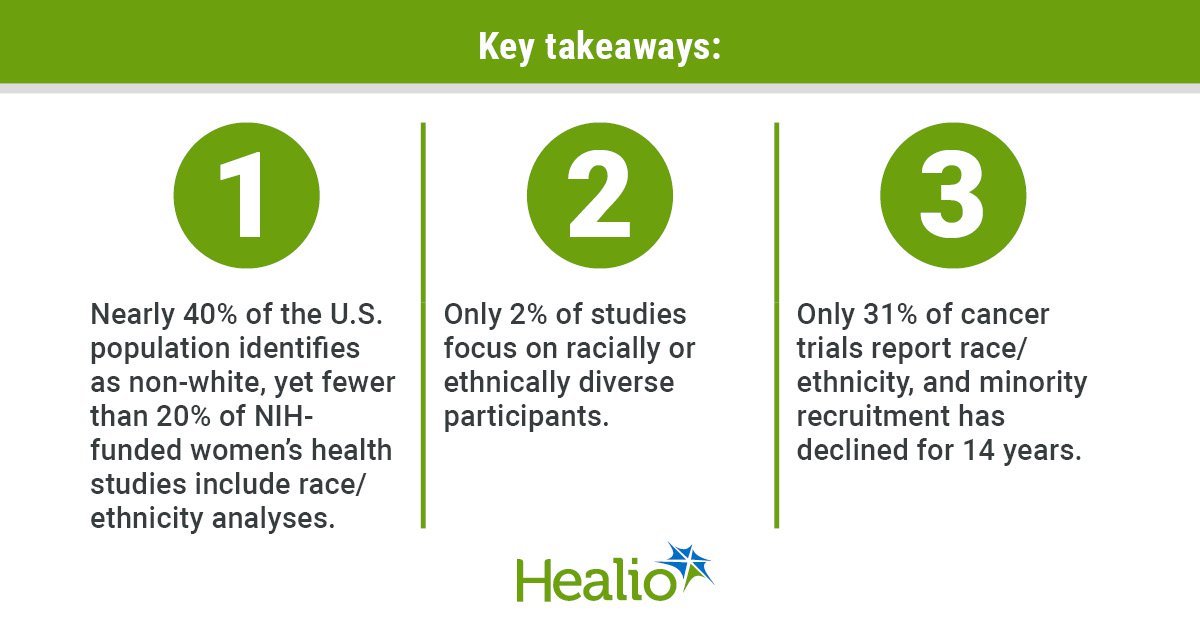
Nearly 40% of individuals in the U.S. identify as a race or ethnicity other than white. However, less than 20% of NIH-funded women’s health research includes race or ethnicity analyses, with only 2% focusing on racially or ethnically diverse participants.
Additionally, race and sex are rarely used as selection criteria.
For cancer trials, recruitment of minorities has continuously decreased over the past 14 years, with only 31% of trials even reporting race or ethnicity.
“This gives new meaning to the saying ‘out of sight, out of mind.’ It is virtually impossible to address a disparity you cannot see,” Prendergast said. “This persistent lack of inclusion has created an environment where our protocols are not generalizable to the entire treatable population.”
Funding disparities continue to bolster this divide. Only about a third of NIH research grants go to women and less than 5% of those go to women of color.
According to Prendergast, lack of mentorship also plays a key role in ongoing disparities, as women, and especially women of color, are less likely to receive the kind of guidance that supports early career physicians, fosters collaboration and paves the way to success.
Disparities in research and care subsequently have profound consequences for women, particularly women of color. Provider bias and perceived discrimination create barriers to open communication, leading patients to be viewed as disengaged or difficult, reinforcing stereotypes and contributing to negative outcomes.
“Harm is inevitable,” Prendergast said. “Inclusion is not optional. It’s fundamental to achieve what we want, which is the best outcomes for everyone.”
She went on to encourage women and allies to use their voices to drive change in research and health care, emphasizing that everyone has a role in closing the gaps that leave women and women of color invisible in clinical trials and health care systems.
“As scientists, we have a seat at the table and we have an opportunity to be a part of the solution — not just a contributor to the problem,” Prendergast said.