August 08, 2025
4 min read
Key takeaways:
- The risk for lung cancer was heightened among those with vs. without ILD in a model that adjusted for five covariates.
- This continued in sibling-controlled analyses of patients with ILD and siblings without ILD.
Individuals with vs. without interstitial lung disease faced an elevated risk for lung cancer and histological subtypes of lung cancer in adjusted and sibling-controlled analyses, according to results published in JAMA Network Open.

Weimin Ye
“Patients with ILD are at an elevated risk of developing lung cancer across all subtypes, especially rare and aggressive forms such as small cell lung cancer, which often has a poor prognosis,” Weimin Ye, MD, PhD, professor in the department of medical epidemiology and biostatistics at Karolinska Institutet, told Healio.

Data were derived from Xu H, et al. JAMA Netw Open. 2025;doi:10.1001/jamanetworkopen.2025.19630.
“This suggests that clinicians should adopt more comprehensive lung cancer screening approaches in ILD patients, including imaging combined with blood-based cancer biomarkers, to improve early detection,” he continued.
In a prospective cohort study using data from the Swedish Total Population Register and Swedish Multi-generation Register, Ye and colleagues assessed 5,425,976 individuals to determine if ILD impacts the risk for lung cancer and individual histological subtypes.
This population was made up of 14,624 individuals with ILD (58.1% men; 65.9% aged older than 40 years) and 5,411,352 individuals without ILD (51.2% men; 24.1% aged older than 40 years), according to the study.
Between the two sets of individuals, researchers found a higher incidence rate of lung cancer over a 30-year follow-up period in the ILD group (355.4 per 100,000 person-years vs. 26.2 per 100,000 person-years).
The study further reported that the risk for lung cancer was heightened among those with vs. without ILD (adjusted HR = 2.16; 95% CI, 1.89-2.46) in a model that adjusted for five covariates: sex, age, calendar period, educational attainment and smoking-related diseases.
Researchers also noted that the ILD group had a heightened risk for lung cancer in an analysis that only included those without smoking-related diseases (HR = 3.68; 95% CI, 3.07-4.41).
Among those with ILD, the incidence rate of lung cancer was greater in the group with vs. without smoking-related diseases (659.6 per 100,000 person-years vs. 247.9 per 100,000 person-years).
Among those without ILD, the incidence rate of lung cancer continued to be higher in the group with vs. without smoking-related diseases (237.1 per 100,000 person-years vs. 20.3 per 100,000 person-years).
“Our results show that individuals with both ILD and smoking-related diseases have the highest risk of developing lung cancer compared to those with only one of these conditions,” Ye told Healio.
“This underlines the critical importance of smoking cessation. Clinicians should strongly encourage ILD patients to quit smoking immediately upon diagnosis to help reduce their cancer risk,” he said.
In each subgroup of sex (men and women), age (< 20 years, 21-40 years and > 40 years), educational attainment (0-9 years, 10-12 years and > 12 years) and follow-up length (1 to < 3 years, 3 to < 6 years, 6 to < 10 years and at least 10 years), those with vs. without ILD had a higher risk for lung cancer; however, only age and follow-up length findings reached significance.
According to the study, the elevated risk for lung cancer associated with ILD was greater in individuals aged younger than 20 years (aHR = 11.26; 95% CI, 3.48-36.38) vs. older than 40 years (aHR = 2.14; 95% CI, 1.85-2.48; P = .02), as well as during 1 to less than 3 years follow-up (aHR = 19.32; 95% CI, 6.91-53.99) vs. at least 10 years of follow-up (aHR = 2.08; 95% CI, 1.51-2.88; P < .001).
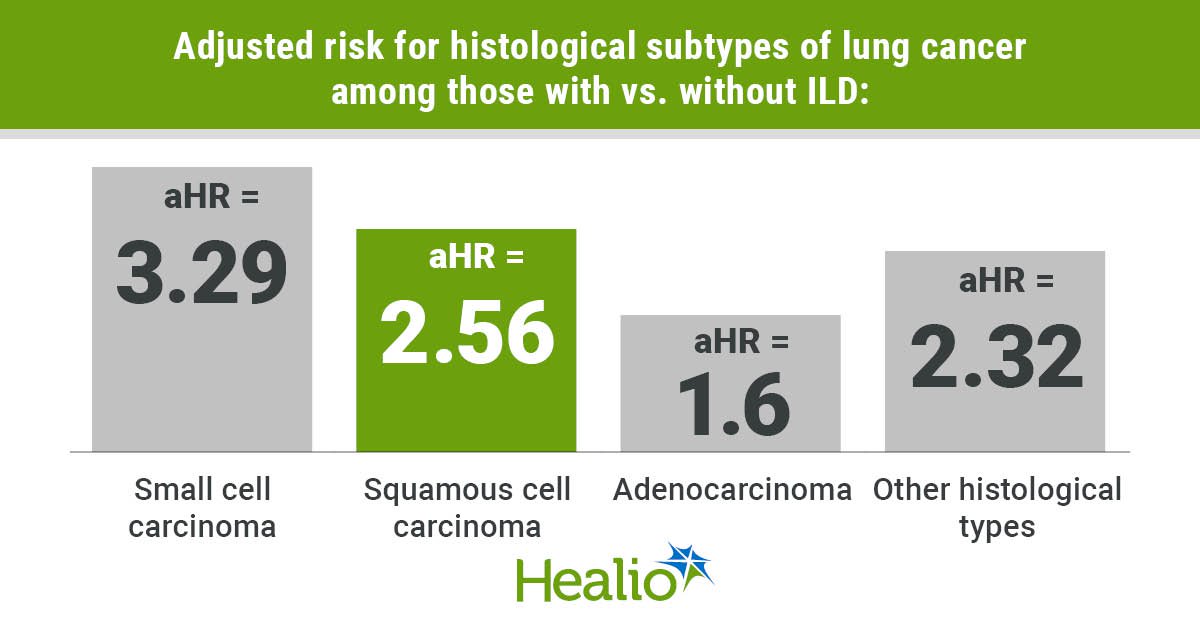
When broken down into histological subtypes of lung cancer, researchers found significantly higher risks in the ILD vs. no ILD group, with the greatest risk reported for small cell carcinoma (aHR = 3.29; 95% CI, 2.32-4.68), followed by squamous cell carcinoma (aHR = 2.56; 95% CI, 1.99-3.29) and adenocarcinoma (aHR = 1.6; 95% CI, 1.28-2.01). The risk for “other histological types” was also heightened in the ILD group (aHR = 2.32; 95% CI, 1.78-3.01).
The above outcomes continued in sibling-controlled analyses of 9,157 individuals with ILD and 21,725 siblings without ILD, according to the study. Those with vs. without ILD faced a significantly raised risk for lung cancer (aHR = 2.91; 95% CI, 1.98-4.27), small cell carcinoma (aHR = 8.09; 95% CI, 2.16-30.38), squamous cell carcinoma (aHR = 2.31; 95% CI, 1.1-4.84), adenocarcinoma (aHR = 2.11; 95% CI, 1.19-3.76) and “other histological subtypes” (aHR = 4.18; 95% CI, 1.64-10.67).
“Given that both ILD and lung cancer are associated with genetic predispositions, we initially hypothesized that adjusting for genetic risk factors, through using sibling-controlled study design, would reduce the observed hazard ratio,” Ye told Healio. But results showed the opposite, he continued, with a persistent robust association between ILD and lung cancer risk and an even higher hazard ratio even after controlling for genetic factors.
“This suggests that non-genetic mechanisms — such as environmental exposures, inflammation or other shared pathophysiological pathways — may play a more dominant role in this link than previously assumed,” Ye said.
Those with vs. without ILD in the sibling-controlled cohort also had a heightened risk for lung cancer in each studied subgroup, but researchers wrote that none reached significance.
“We believe that future studies should focus on elucidating the underlying mechanisms linking ILD with different histological subtypes of lung cancer,” Ye told Healio. “This line of research may provide deeper insights into the pathogenesis of lung cancer and help identify subtype-specific pathways, which could ultimately inform more targeted prevention and treatment strategies.”
For more information:
Weimin Ye, MD, PhD, can be reached at weimin.ye@ki.se.