August 21, 2025
4 min read
Key takeaways:
- HPV testing rates in oropharyngeal cancer have increased over time but remain suboptimal.
- Testing uptake varies by patient race, socioeconomic factors, treatment setting and disease subtype.
HPV testing in oropharyngeal cancer remains substandard despite recommendations for universal adoption, according to results of a cross-sectional study.
Testing rates have increased over time, but uptake varies by patient race, socioeconomic factors, treatment setting and disease subtype.

Data derived from Carlson KM, et al. JAMA Netw Open. 2025;doi:10.1001/jamanetworkopen.2025.23917.

Angela L. Mazul
“HPV status is very important in oropharyngeal cancer, both for prognostication and clinical trial eligibility,” researcher Angela L. Mazul, PhD, MPH, assistant professor in the department of otolaryngology at the University of Pittsburgh and UPMC Hillman Cancer Center, told Healio. “The fact that a sizable proportion of patients are not tested, and there are disparities in who gets tested and who doesn’t, is problematic.”
Identifying gaps
Oropharyngeal squamous cell carcinoma (OPSCC) is the most common HPV-associated malignancy in the United States.
Incidence increased by 0.8% per year among women and 2.7% among men from 1999 to 2015, according to study background.
Approximately 58,500 people will be diagnosed with OPSCC this year and more than 12,250 people will die of the disease, according to The Oral Cancer Foundation.
HPV status provides considerable prognostic value in OPSCC.
A landmark study published in 2010 showed individuals with HPV-positive disease achieved considerably better 3-year survival than those with HPV-negative disease (82.4% vs. 57.1%). Data adjusted for race, ethnicity, age, tumor stage, tobacco use and other factors revealed a 58% reduction in mortality risk among those with HPV-positive disease.
In 2012, National Comprehensive Cancer Network recommended universal HPV testing for patients with OPSCC.
Six years later, the eighth edition of the American Joint Committee on Cancer (AJCC) Staging Manual incorporated HPV status — as determined through p16 immunohistochemical analysis — into OPSCC staging. This resulted in some HPV-positive OPSCC cases that had been classified as stage III or stage IV being reclassified to earlier stages given the traditionally improved outcomes for patients with HPV-positive disease.
Two studies conducted prior to the AJCC update showed suboptimal HPV testing rates, particularly among racial or ethnic minority individuals and other underserved populations. However, no studies have evaluated testing trends since 2018.
“If you don’t test for HPV, you can’t give an accurate prognosis,” Mazul said. “There also are clinical trials evaluating whether we can scale back treatment for HPV-positive cancers to reduce toxicity and improve quality of life, so it’s very important that we assess the trends and see if there are gaps that need to be addressed.”
Insufficient progress
Mazul and colleagues — including first author Katie M. Carlson, MPH, an epidemiologist at University of Pittsburgh and UPMC Hillman Cancer Center — used the National Cancer Database to evaluate HPV testing rates and specific factors among patients diagnosed with OPSCC between 2013 and 2021.
The researchers also assessed whether specific factors contributed to uptake. They stratified results by clinical factors (eg, year of diagnosis, disease stage and facility type) and sociodemographic factors (eg, sex, age, race/ethnicity, insurance type and income/education levels in their ZIP code).
The analysis included 135,756 patients (86.2% white; 83.4% male) divided into two cohorts based on year of diagnosis.
One cohort included 70,911 patients (82.9% male) diagnosed between 2013 and 2017. During the 5-year period, 71.2% of patients underwent HPV testing and 28.8% did not. Nontesting rates declined from 36.4% in 2013 to 21.9% in 2017.
The other cohort included 64,845 patients (83.9% male) diagnosed between 2018 and 2021.
During the 5-year period, 92.8% of patients underwent HPV testing and 7.2% did not. Nontesting rates declined from 8.9% in 2018 to 6.3% in 2021.
Multivariable analysis of results from the 2018-2021 cohort identified several factors associated with testing uptake.
Results showed higher nontesting rates among:
- patients of Black race (prevalence ratio [PR] = 1.18; 95% CI, 1.05-1.33) or other race (PR = 1.39; 95% CI, 1.17-1.66) compared with white patients;
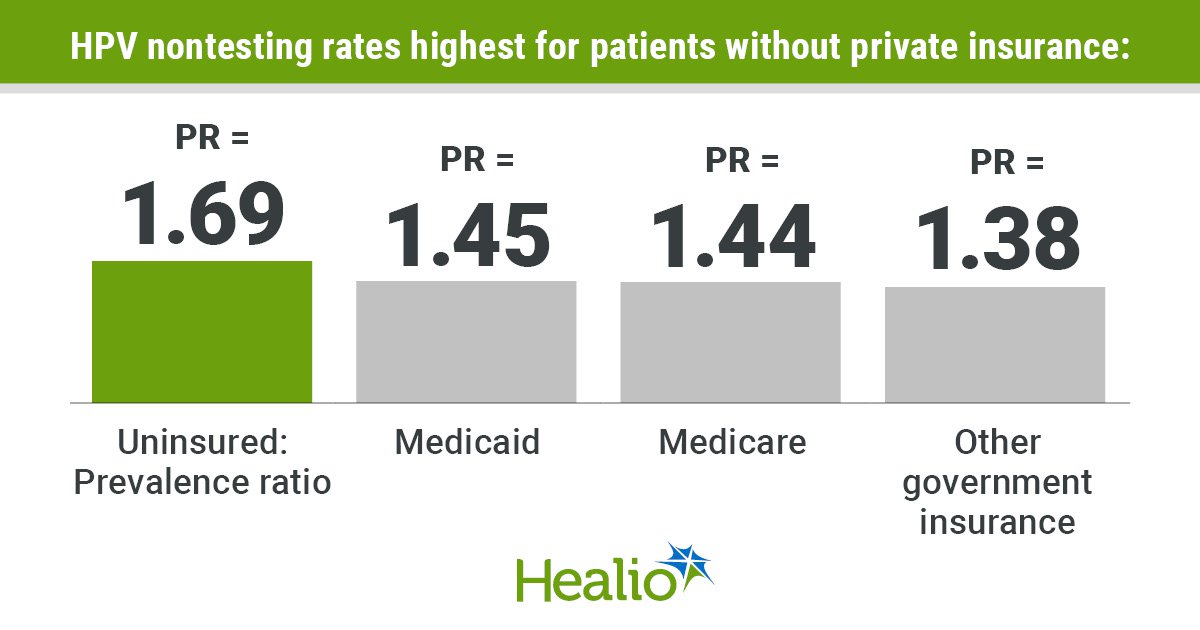
- uninsured patients (PR = 1.69; 95% CI, 1.42-2), those with Medicaid (PR = 1.45; 95% CI, 1.29-1.62), Medicare (PR = 1.44; 95% CI, 1.34-1.55) or those with other government insurance (PR = 1.38; 95% CI, 1.16-1.66) compared with those with private insurance or managed care;
- patients diagnosed at integrated network (PR = 1.17; 95% CI, 1.06-1.28), comprehensive community (PR = 1.2; 95% CI, 1.11-1.29) or community cancer programs (PR = 1.36; 95% CI, 1.2-1.54) compared with those diagnosed in research or academic programs; and
- patients with base-of-tongue subsite (PR = 1.83; 95% CI, 1.7-1.97) or other subsite (PR = 1.78; 95% CI, 1.63-1.95) compared with those who had tonsil subsite.
More research is needed to better understand reasons for variations in testing, Mazul said. However, structural challenges and implicit bias may both contribute.
“Perhaps the hospitals where these patients go don’t have the resources,” she said. “HPV-positive cancers also are more common among white individuals with higher socioeconomic status, so that may make some clinicians less likely to test patients of other races if they believe they are less likely to have HPV-positive disease. But by doing that, you’re not able to fully prognosticate and you’re also withholding shared decision-making from the patient.”
The researchers acknowledged study limitations, including the potential for selection bias and the fact income and educational attainment levels in the National Cancer Database are established at the ZIP code level rather than the individual level. Also, patients with unknown HPV testing status were included in the nontesting category, so it is possible some of those patients had been tested.
Still, the findings highlight the need for greater scrutiny of HPV testing practices, as well as the need for more research into the barriers that must be overcome to achieve better compliance with testing guidelines, the researchers concluded.
“HPV testing is easy, inexpensive and covered by most insurances, yet we’re still seeing disparities,” Mazul said. “That is important to keep in mind as we continue to identify new biomarkers and move forward with molecular genomics. We have to make sure vulnerable populations can still access these very important types of prognostication.”
References:
For more information:
Angela L. Mazul, PhD, MPH, can be reached at angela.mazul@pitt.edu.