Lacerations to the hand are common injuries that present to emergency departments, both in academic Level I trauma centers as well as community and rural settings. Lacerations across the dorsal surface of the hand and fingers often injure the extensor tendons of the fingers, leading to difficulty or inability to extend the joints of the finger.
The repair of these tendons is essential to preserving function of the hand and can be performed by a hand surgeon, but it is a relatively simple procedure, and in a resource-limited setting, can be performed by an emergency physician.
For a brief review of the anatomy and physiology of the extensor tendons, the tendons from muscles of the forearm meet the tendons of the hand in a sheet at the base of each finger (near the knuckle). The extensor digitorus communis (EDC) muscle of the forearm supplies tendons that work to extend the index, middle, ring, and small fingers. The index finger has two tendons (EDC and extensor indices proprius). The extensor digiti minimi muscle (EDM), in addition to the EDC, works in conjunction to extend the fifth digit. The extensor pollicis brevis and longus muscles supply the tendons for the thumb. The sheet of tendinous material gives off a central band that extends the middle joint of the finger, and two separate lateral bands that converge together past the joint and function to extend the distal interphalangeal (DIP) joint. Unlike flexor tendons, extensors usually do not retract significantly because of connections called juncturae tendinae.
To diagnose an extensor tendon injury, the patient will have pain with, or an inability to extend, one of the joints of the finger or finger drooping. Traumatic etiology of extensor tendon injury involves penetrating or blunt trauma to or with extension to the dorsal surface of the wrist, hand, or finger.
Once diagnosed, repair can be attempted. To prepare for the procedure, use a blood pressure cuff around the forearm and inflate it to 50 mmHg above systolic pressure to control bleeding. You can achieve anesthesia with digital ring block, local anesthetic, or systemic analgesia or moderate sedation, as needed. Liberally irrigate site of injury with 500 mL to 1 L of normal saline and apply sterile drapes around site of procedure.
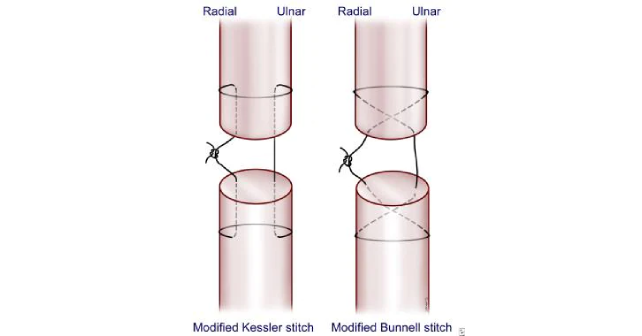
The repair is performed by extending the site of injury to visualize both ends of the severed tendon and using sutures to join the cut ends together. For injuries to the extensor tendon when it travels through the hand or proximal finger, the Modified Kessler stitch or Modified Bunnell stitch can be used (see Image 1).
To perform a Modified Kessler stitch: Insert the needle perpendicular to the proximal severed surface of tendon along the radial side (closest towards thumb), then exit the tendon laterally and wrap the string around the tendon. Insert the needle into the ulnar side of the tendon at approximately the same distance from the lacerated edge where the needle pierced the radial side, then exit the tendon perpendicularly through the severed end of tendon at a 90-degree angle. Now join the proximal tendon with the distal tendon by entering the distal tendon severed surface on ulnar side, exit out the tendon laterally, wrap around the tendon, and reenter the distal tendon on radial side, exiting through severed surface on radial half. Tighten the string and tie a knot that will be buried between the two segments of tendon.
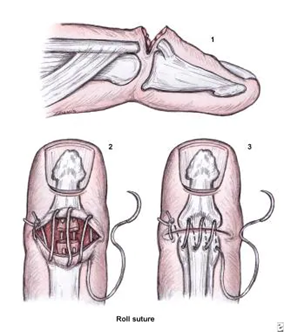
To perform a Modified Bunnell stitch: Injury to the tendon at the distal finger near the DIP joint should be repaired by dermatotenodesis (see Image 2). This is performed by anchoring a simple suture on one end of the skin incision, leaving the tail of the suture long enough to perform the rest of the repair. Then perform running sutures until you reach the area where the tendon is located, and upon reentering skin on the distal end of the laceration, take a bite into the superior surface of distal tendon on its lateral side (⅓ through diameter), exiting out through severed surface of the distal tendon. Enter the proximal tendon through the lateral aspect of the severed surface, and exit out through the superior surface, also grabbing overlying skin. Repeat this technique by reentering the skin that is overlying medial ⅓ tendon and grabbing distal and proximal tendon fragments, exiting out through the skin. Place a single suture at the medial end of the incision to anchor the skin.
For all repairs, apply a volar splint to keep the affected tendon and joints held in extension for at least six weeks, making sure that the dressing isn’t too tight and the fingers are well perfused. Refer the patient to a hand surgeon or orthopedic surgeon for follow up. The splint pictured here can be used for injuries to the tendon at the distal finger involving DIP joint (repaired using dermatotenodesis).
Common complications after extensor tendon repair include infection, adhesions resulting in decreased mobility of hand, mallet deformity or swan neck deformity of finger, or ulceration to skin from splint application.
 Dr. Dooley is an assistant professor of emergency medicine at Baylor College of Medicine in Houston, Texas.
Dr. Dooley is an assistant professor of emergency medicine at Baylor College of Medicine in Houston, Texas.
Dr. Smith is an assistant professor of plastic surgery at the University of Texas Medical Branch.
- The British Society for Surgery of the Hand. Extensor tendon injury. 2017. (n.d.). The British Society for Surgery of the Hand. https://www.bssh.ac.uk/patients/conditions/27/extensor_tendon_injuryh https://www.bssh.ac.uk/patients/conditions/27/extensor_tendon_injury.
- Baecher, N. B. (2023). Extensor Tendon Repair Technique. MedScape. 2023.
- The American Society for Surgery of the Hand.https://www.assh.org/handcare/safety/tendons#Finger%20Extensor