August 05, 2025
6 min read
Key takeaways:
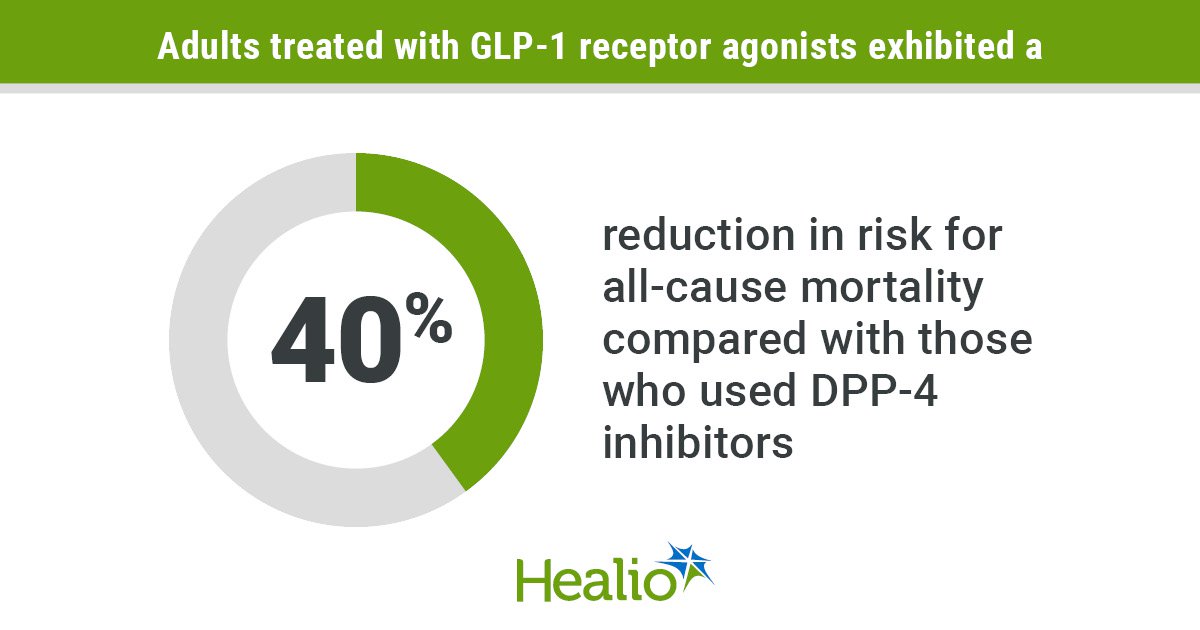
- GLP-1 receptor agonists reduced mortality vs. DDP-4 inhibitors among older adults with cancer and type 2 diabetes.
- More patient-clinician communication about GLP-1 therapy risks and benefits is needed.
Choice of therapy to control high blood sugar may affect survival among older adults with cancer and type 2 diabetes, according to study results.
Those who used GLP-1 receptor agonists exhibited significantly lower risk for all-cause mortality than those treated with dipeptidyl peptidase-4 (DPP-4) inhibitors. Results showed comparable mortality risks between users of GLP-1 agents and sodium-glucose transport protein 2 (SGLT2) inhibitors.

Data derived from Radwan RM, et al. JAMA Netw Open. 2025;doi:10.1001/jamanetworkopen.2025.21887.
The data — which support findings of prior investigations — add to evidence that can help guide treatment decisions, according to senior author Jiang Bian, PhD, MS, FACMI, associate dean for data science at Indiana University School of Medicine.
“GLP-1s and SGLT2s have different mechanisms, so the question of whether to use an SGLT2 comes down to what condition you are managing,” Bian, who also serves as chief data scientist for IU Health and Regenstrief Institute, told Healio. “Newer GLP-1s are more expensive, so cost also may be a factor.”
Despite increased adoption of GLP-1 medications for multiple indications, more communication between patients and health care providers about these agents is necessary, results of a second study revealed.
A review of social media posts about GLP-1 therapies showed concerns about whether they raise cancer risk persist — particularly among cancer survivors or those with a family history of cancer — but a considerable percentage of individuals do not appear to be discussing those concerns with their clinicians.
“These medications often are used for weight loss, and that topic still carries a sort of stigma,” Ramez Kouzy, MD, radiation oncology resident at The University of Texas MD Anderson Cancer Center, said in an interview. “That may make a person more inclined to ask questions online rather than bringing them up to us in clinic.
“However, we know not everything online is fact-checked or of scientific merit,” Kouzy added. “If physicians don’t know the types of questions patients are asking, and if we’re not proactively seeking that information, they may be more likely to resort to online forums or other mediums with questionable data.”
Survival benefits
GLP-1 receptor agonists can reduce glucose, decrease inflammation and improve insulin resistance, three factors linked to cancer progression.
However, the effects of these medications and other glucose-lowering drugs on cancer survival have not been well established.
Bian and colleagues conducted a retrospective cohort study to assess whether use of GLP-1 receptor agonists instead of other glucose-lowering medications improved survival for older adults with cancer and type 2 diabetes.
The researchers used Medicare data from 2013 to 2020 to identify adults aged 66 years or older who had type 2 diabetes and one of nine cancer types — bladder, breast, colorectal, endometrial, kidney, lung, pancreatic, prostate or thyroid.
All adults initiated one of three types of glucose-lowering drugs — GLP-1 receptor agonists, DPP-4 inhibitors or SGLT2 inhibitors — and survived at least a year after cancer diagnosis.
Follow-up continued from the time of first drug prescription until death or Dec. 31, 2020. Researchers used 1:1 propensity score matching to minimize confounding in their survival analyses.
One cohort established to compare outcomes between users of GLP-1 receptor agonists and SGLT2 inhibitors included 2,553 matched pairs (mean age, 73.9 years; 56% men, median follow-up, 1.65 years). Another cohort established to compare outcomes between users of GLP-1s and DPP-4 inhibitors included 2,564 matched pairs (mean age, 74.1 years; 53.1% men; median follow-up, 1.73 years).
Results showed no difference in mortality risk between individuals who used GLP-1s vs. SGLT2 inhibitors (HR = 1.03; 95% CI, 0.85-1.23).
However, researchers observed significantly lower all-cause mortality among individuals who used GLP-1 medications vs. those who used DPP-4 inhibitors (HR = 0.6; 95% CI, 0.51-0.7). Subgroup analyses showed the benefit with GLP-1s persisted regardless of sex, age and obesity status.
Analysis by race/ethnicity revealed a significant survival benefit only for non-Hispanic white individuals (HR = 0.61; 95% CI, 0.51-0.74). Analysis by cancer type showed significant benefit for those with lung (HR = 0.3; 95% CI, 0.16-0.56), colorectal (HR = 0.33; 95% CI, 0.17-0.63) or breast cancers (HR = 0.6; 95% CI, 0.41-0.89).
Researchers acknowledged study limitations, including potential residual confounding and small sample sizes in some subgroup analyses.
A KFF Health Tracking Poll released last year indicated about 12% of U.S. adults had used a GLP-1 agonist. However, these agents still are relatively new, and their long-effects will be important to study, Bian said.
“Most of the knowledge we have comes from real-world evidence, but there is still debate in some disciplines about the value of that,” he said. “Randomized controlled trials are the gold standard, but they are very expensive — especially if you’re looking at long-term outcomes. If we can use this real-world evidence and identify particular hypotheses of interest that can be used to design randomized trials, that would be very helpful.”
Communication gaps
Most experimental and observational studies show GLP-1 receptor agonists do not increase overall cancer risk, according to a systematic review by Lin and colleagues published earlier this year.
However, risk profiles vary based on specific cancer types, with some reports linking GLP-1 medications to higher risks for thyroid cancer or pancreatic cancer.
The FDA has advised individuals with personal or family history of medullary thyroid cancer to avoid semaglutide — the active ingredient in Ozempic (Novo Nordisk) and Wegovy (Novo Nordisk) — and tirzepatide (Zepbound, Eli Lilly & Co.).
Kouzy and colleagues conducted a cross-sectional study that examined how patients discuss cancer-related risks of GLP-1s on social media, as well as the level of patient-clinician communication about these risks.
Researchers analyzed posts and comments from the five most active Reddit forums related to GLP-1 medications.
They extracted 410,710 unique entries, filtered them using prespecified keywords related to cancer, and then used an AI-assisted approach to help extract key variables such as cancer survivorship, risk perceptions and physician discussions.
Their analysis included 1,529 posts — from 1,067 unique users — that discussed cancer-related topics.
The most common cancer types mentioned included thyroid cancer (26.3%) and breast cancer (9.5%).
Cancer survivors wrote 409 (26.7%) of the cancer-related posts, and 146 (35.7%) of those posts mentioned use of GLP-1 receptor agonists for weight management during survivorship.
People with a family history of cancer wrote 239 (15.6%) of the cancer-related posts.
About half (51.3%; n = 784) of the posts included in the analysis discussed the effects of GLP-1 agents on cancer risk; however, only one in five posts (19.2%; n = 293) mentioned discussing these risks with physicians.
Three times as many social media posts analyzed expressed concern about the potential for GLP-1 medications to increase cancer risk (20.9%; n = 319) vs. their potential to reduce risk for future obesity-related cancers (6.5%; n = 100).
Researchers acknowledged study limitations, including self-selection bias on social media — and the potential that these individuals may represent more extreme views —and the possibility that the AI extraction pipeline may have interpreted nuanced content.
This study can “open the door” for researchers to study GLP-1 medications in specific patient populations such as cancer survivors, Kouzy said.
The findings also highlight the need for more patient-clinician communication about cancer risks associated with GLP-1 medications, Kouzy said.
“Hopefully this study can help health care professionals better understand the types of information people are seeking online so they can educate themselves and be better prepared to have these conversations with their patients,” Kouzy said. “It’s also OK for oncologists to say ‘I don’t know’ and refer our patients to endocrinologists or the prescriber of GLP-1 medications, particularly for questions about their side-effect profile.”
Health care providers should proactively initiate the discussions, especially with cancer survivors and other individuals at higher risk, Kouzy said.
“It comes down to having a clear, open line of communication,” Kouzy said. “This is not a static message that applies across the general population. This is an evolving conversation. If you know your patient is using this type of medication, you should encourage them to be open about it and educate yourself so you can formulate personalized recommendations for the patient in front of you.”
References:
For more information:
Jiang Bian, PhD, can be reached at bianji@iu.edu.
Ramez Kouzy, MD, can be reached at rkouzy@mdanderson.org.