October 06, 2025
2 min read
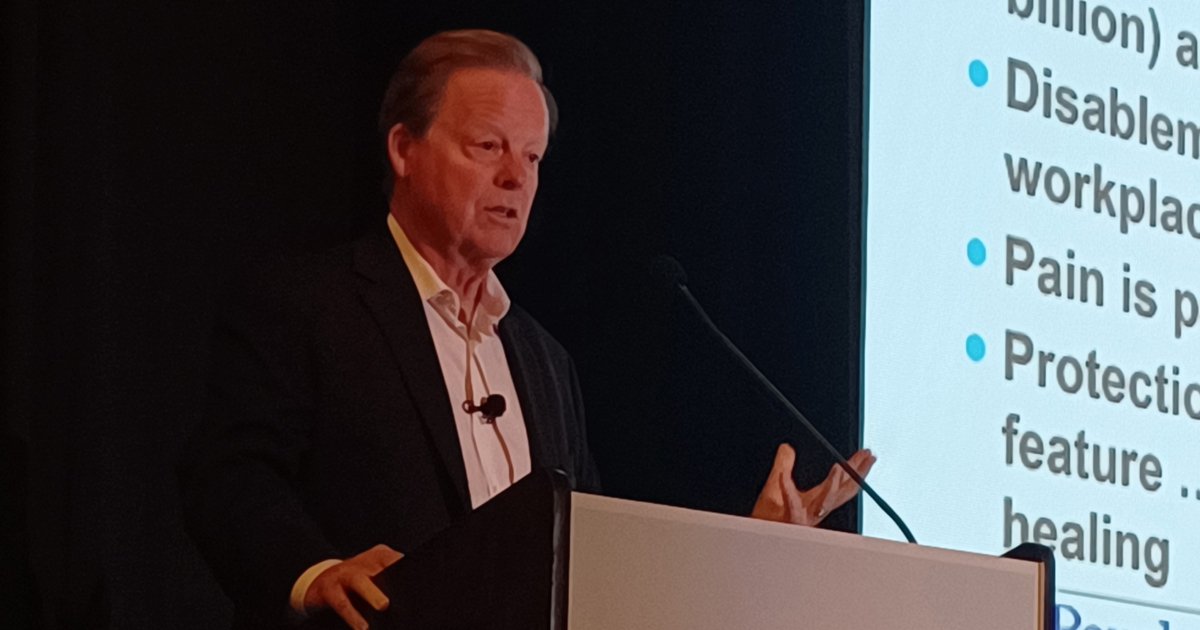
HUNTINGTON BEACH, Calif. — Chronic pain is too complex for “linear” approaches and instead requires an interdisciplinary focus on behavioral and physical health, said a presenter at the 2025 Congress of Clinical Rheumatology West.
“As rheumatologists, you are acutely aware that your patients come in very complex — no simple patient comes into rheumatology, or pain medicine by the way,” said Martin D. Cheatle, PhD, director of behavioral medicine for the Penn Pain Medicine Center, at the University of Pennsylvania Perelman School of Medicine. “These patients typically have chronic pain, which brings with it its own host of problems, but also psychiatric and psychological medical comorbidities.

“No matter how brilliant you are with pharmacotherapy, it can’t have the same impact as looking at the whole person,” said Martin D. Cheatle, PhD. Image: Jason Laday | Healio Rheumatology.
“And to be effective as a clinician, you have to have a broader lens on how you approach these patients, which is what I’m going to try to convince you is the biopsychosocial model of care,” he added.
According to Cheatle, the current approach to pain management remains “linear in nature,” in which symptoms lead to a diagnosis and then to treatment.
However, Cheatle argued that chronic pain is a complex condition flush with multiple medial and psychiatric comorbidities. As such, a more “expansive and holistic” approach is required to increase the potential for improved outcomes.
“You look at outcomes studies for chronic pain: they’re all poor,” he said. “Opioid therapy, non-opioid therapy, pharmacotherapy, injection therapy, implantable devices, surgery, and even spinal cord stimulators for neuropathic pain has a shelf life of about 3 years before it starts losing its effectiveness.”
Cheatle instead counseled the use of the biopsychosocial model of care. The four planks of this model are:
- building a therapeutic relationship with the patient in the initial encounter;
- diagnostic evaluation, including an interview, physical examination and imaging;
- mental health, sleep and substance use disorder assessments; and
- treatment, drawing together cognitive behavioral therapy, pharmacotherapy, graded exercise, nutritional counseling and weight loss if needed, and social support.
Cheatle additionally stressed the importance of interdisciplinary care vs. multidisciplinary care. In a multidisciplinary model, several disciplines may be involved, but they often lack coordination, he said. They act in parallel and often with different goals.
Meanwhile, in an interdisciplinary model, team members hold complementary roles, actively collaborate and arrive at treatment decisions based on consensus.
“Pain is complex; you cannot attack it from a linear perspective,” said Cheatle. “No matter how brilliant you are with pharmacotherapy, it can’t have the same impact as looking at the whole person.
“Managing pain is particularly challenging,” he added. “Patients suffering from any type of chronic pain require an interdisciplinary team. You’re going to have to cobble this together. Wherever you are in your community, try to find a physical therapist or two who see this as a challenge. Find a mental health provider who finds this challenging, and who is willing to try to use some of these interventions. There is also a need for specific changes in reimbursement policies to support care and cognitive medicine. People need to be paid more for thinking.”
For more information:
Martin D. Cheatle, PhD, can be reached at rheumatology@healio.com.