[ad_1]
October 03, 2025
4 min read
Key takeaways:
- Vomiting and fatigue were among patient-reported symptoms linked to ED visits and hospitalizations during chemotherapy.
- Multiple symptoms on same day significantly raised the odds of unplanned health encounters.
Daily tracking of moderate to severe symptoms such as vomiting and fatigue between chemotherapy visits could help identify individuals who have a higher likelihood of visiting the ED or requiring inpatient care.
A longitudinal evaluation of patient-reported outcomes found several symptoms had a significant association with patients going to the ED or being hospitalized within the following week, and having multiple symptoms on the same day greatly increased the likelihood of these unplanned health encounters.

Data derived from Kairis E, et al. JCO Oncol Pract. 2025;doi:10.1200/OP-25-00177.

Carissa A. Low
“There’s a lot that’s missed in terms of what providers see,” Carissa A. Low, PhD, associate professor of hematology/oncology and psychology at University of Pittsburgh, told Healio.
“If they’re only getting eyes on patients every few weeks, and only hearing from patients when something rises to the level of severity where the patient feels motivated to make a phone call, they might be missing a lot of things that could potentially be managed earlier and on an outpatient basis. There’s value to having more frequent assessments.”
‘A lot of value’
Many individuals undergoing chemotherapy end up going to the ED or are hospitalized due to treatment-related adverse events, yet more than half of ED visits could be prevented, according to study background.
Patients frequently report gastrointestinal symptoms and pain in the ED, but those problems could be managed in an outpatient setting with more timely interventions.
Patient-reported outcomes could help inform health care teams of developing toxicities prior to ED visits or inpatient treatment.
“We think there’s a lot of value to that data,” Low said. “We were hoping to find that there was utility in asking patients about their symptoms more frequently than is commonly done. We know things can change pretty quickly during chemotherapy and other cancer treatments. We thought that having more daily, frequent assessments would help us pick up on things heading on a downward trajectory faster, which might give clinicians more of an opportunity to intervene earlier.”
Researchers enrolled 183 adults (mean age, 59.49 years; standard deviation, 11.87; 61.7% women; 79.8% white; 36.1% gastrointestinal cancer) receiving chemotherapy for any solid tumor at UPMC Hillman Cancer Center.
Participants completed a daily questionnaire on their smartphones rating 16 symptoms: abdominal pain, anxiety, concentration issues, constipation, decreased appetite, diarrhea, dizziness, fatigue, insomnia, nausea, neuropathy, pain, problems with memory, sad or unhappy feelings, shortness of breath, and vomiting.
They rated frequency, severity and/or interference of those symptoms 0 to 4 during the 90-day study.
Unplanned health encounters, defined as an ED visit or inpatient hospitalization, within 7 days of a symptom served as the primary endpoint.
Multiple symptoms have significant associations
In all, 32.8% of patients had unplanned health encounters.
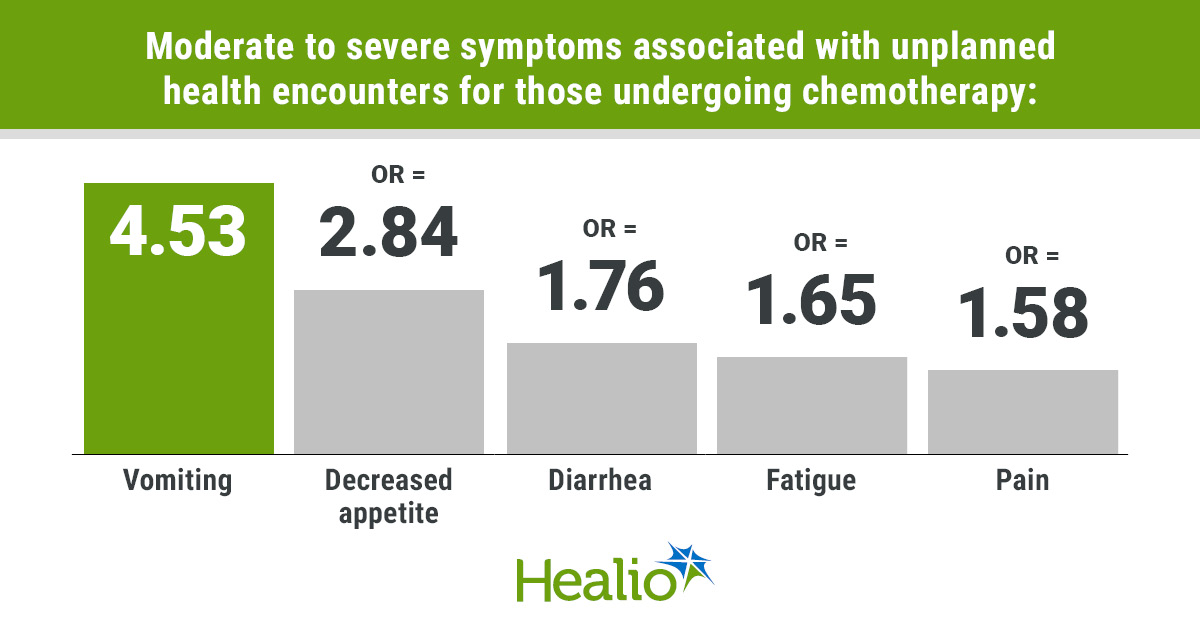
Moderate to severe symptoms that had a significant association with unplanned health encounters within 7 days included vomiting (OR = 4.53; 95% CI, 1.77-11.58), decreased appetite (OR = 2.84; 95% CI, 1.94-4.17), shortness of breath (OR = 2.5; 95 CI, 1.44-4.34), diarrhea (OR = 1.76; 95% CI, 1.11-2.79), fatigue (OR = 1.65; 95% CI, 1.2-2.26) and pain (OR = 1.58; 95% CI, 1.01-2.48).
Each of these symptoms had a significant association with unplanned health encounters after adjusting for days since study enrollment, as did abdominal pain (OR = 2.17; 95% CI, 1.31-3.58).
“I was surprised to see fatigue pop out because that’s so nonspecific,” Low said. “It’s almost universal during cancer treatment, so we weren’t sure whether we’d see much of a signal there.”
Low and colleagues did not observe a significant association with unplanned health encounters and cognitive or psychiatric symptoms or constipation, dizziness or neuropathy.
Multiple moderate to severe symptoms occurring on the same day significantly increased the odds of an unplanned health encounter compared with days without symptoms, and that risk increased with additional symptoms: two symptoms (OR = 1.97; 95% CI, 1.17-3.32), three symptoms (OR = 2.13; 95% CI, 1.33-3.39) and four or more symptoms (OR = 5.32; 95% CI, 2.91-9.72).
Researchers acknowledged study limitations, including its single-institution design.
Make information ‘more actionable’
Low described the results as “helpful in guiding which symptoms to focus on between clinical visits,” but noted the importance of further research.
Low and colleagues are planning a follow-up study asking patients specifically about the symptoms that had a significant association with unplanned health encounters.
“If we do notice something rising above the level of concern, we will send them notifications, prompting them to consider reaching out to their clinical care team, trying to get more information about how they’re feeling,” Low said. “We’re trying to make this information more actionable and see whether that has any impact on symptom burden, quality of life and other outcomes.”
They also want to evaluate if symptoms are persistent or progressing, which could add “even more clinical context and value,” Low explained.
“Overall, it does seem feasible [for patients to use smartphones to report their own symptoms], especially if they know that clinicians are looking at this information,” Low said.
She described herself as “optimistic” on whether this intervention could be implemented in other clinics.
“It’s really important to check in with patients in between clinical visits,” Low said. “I know that most providers don’t have time to do that, but I think leveraging technology to allow patients to share how they’re feeling could really improve care, communication with providers, help patients feel like more active participants in their care, and maybe help prevent some of these complications and unplanned health care encounters from happening.”
For more information:
Carissa A. Low, PhD, can be reached at lowca@upmc.edu.
[ad_2]
Source link