August 29, 2025
4 min read
Key takeaways:
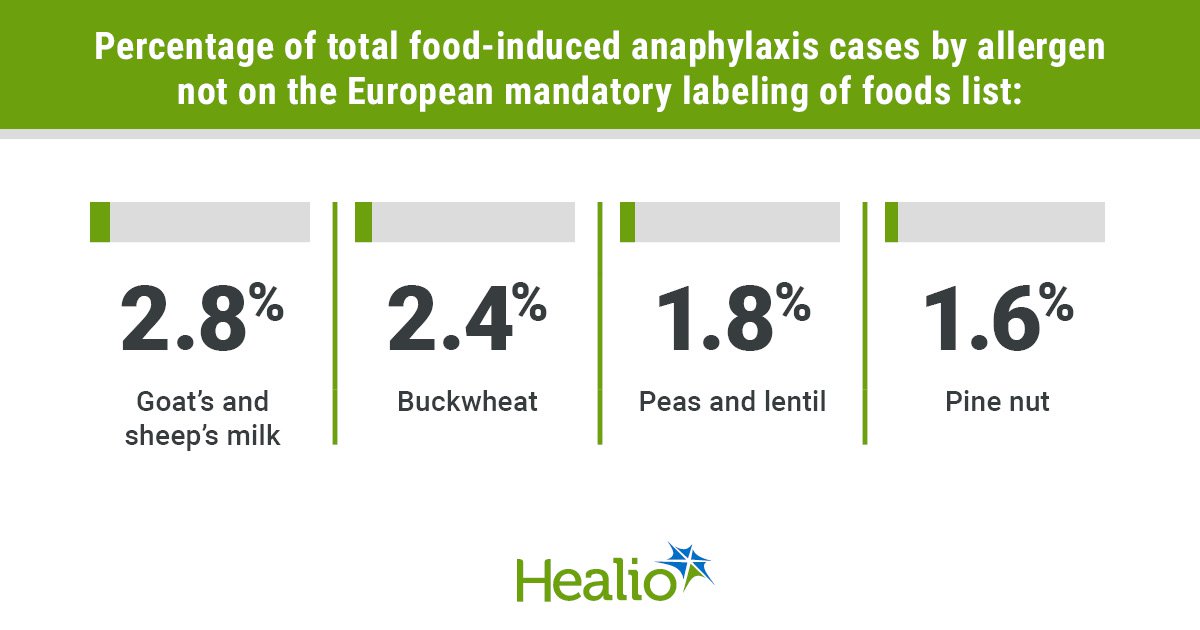
- The four allergens are goat and sheep’s milk, buckwheat, peas-lentils and pine nut.
- The call for mandatory labeling of these allergens is based on frequency, severity, recurrence and hidden exposure prevalence.
Goat’s and sheep’s milk, buckwheat, peas and lentils, and pine nut are allergens that could be added to the European mandatory labeling of foods list based on their presence in cases of severe food anaphylaxis, according to study data.
These findings were published in Clinical & Experimental Allergy.

Data were derived from Sabouraud-Leclerc D, et al. Clin Exp Allergy. 2025;doi:10.1111/cea.70130.

Xavier Van der Brempt
“Our results have a huge impact for clinicians: more than one in seven cases of severe food anaphylaxis are due to an allergen whose labeling is not mandatory,” Xavier Van der Brempt, MD, PhD, pulmonologist, allergist and group leader at Clinique Saint-Luc Bouge in Belgium, told Healio.
“We therefore strongly recommend an urgent review of food labeling legislation in Europe, and probably in other parts of the world,” he continued. “Based on our data, this should at least include goat and sheep milk, buckwheat, peas and lentils, and pine nuts, in addition to the 14 food allergens included in the current list.”
Using 2002 to 2023 data from the Allergy Vigilance Network, Van der Brempt and colleagues evaluated 2,999 cases of food-induced anaphylaxis to determine if there are allergenic foods, besides the 14 already on the European mandatory labeling of foods list, leading to this outcome and deserving of a spot on the list.
“Our allergy monitoring network has been collecting cases of severe anaphylaxis for over 20 years,” Van der Brempt told Healio. “Regarding food allergies, we were surprised to see the high frequency of anaphylaxis linked to food allergens without mandatory labelling, which led us to conduct this study.”
According to the European Union, the 14 foods requiring mandatory labeling are cereals containing gluten (wheat, rye, barley, oats or their hybridized strains); crustaceans; eggs; fish; peanuts; soybeans; milk; nuts (almonds, hazelnuts, walnuts, cashews, pecan nuts, Brazil nuts, pistachio nuts, macadamia or Queensland nuts); celery; mustard; sesame seeds; sulfur dioxide and sulfites “more than 10 mg/kg or 10 mg/L in terms of the total (sulfur dioxide);” lupin; and mollusks.
Researchers found 413 food-induced anaphylaxis cases (13.8%) involving an allergenic food not on the list, and eight foods/food groups were observed in at least 1% of cases.
The food in this set appearing in the greatest proportion of cases was goat’s and sheep’s milk (2.8%; n = 84; 77.4% children). The second most prevalent food involved in food-induced anaphylaxis cases was buckwheat (2.4%; n = 71; 35.2% children), followed by peas and lentil (1.8%; n = 55; 85.5% children), alpha-gal (1.7%; n = 50; 6% children), pine nut (1.6%; n = 49; 73.5% children), kiwi (1.5%; n = 44; 61.4% children), beehive products (1%; n = 30; 16.7% children) and apple (1%; n = 30; 40% children).
Based on the Ring and Messmer anaphylaxis grading scale, researchers reported reactions of the highest severity (grade 4) in four of the above foods/food groups: alpha-gal (8%), goat’s and sheep’s milk (4.8% including two deaths), peas and lentils (1.8%) and buckwheat (1.4%).
Additionally, there were cases with grade 3 reactions in each food/food group, and the study highlighted that the allergen with the highest proportion of individuals with this reaction grade was kiwi (54.5%), followed by alpha-gal (54%), pine nut (49%), apple (46.7%), buckwheat (46.5%), goat’s and sheep’s milk (46.4%), beehive products (33.3%) and peas and lentils (20%).
“The frequency and the severity of the cases were somewhat surprising,” Van der Brempt told Healio.
All eight foods/food groups also resulted in recurrent reactions, according to researchers. The recurrence rate was at least 45% in the allergens of alpha-gal (66%), goat’s and sheep’s milk (56%) and buckwheat (49.3%). This rate did not go above 30% in the remaining allergens: apple (20%), kiwi (27.3%), beehive products (16.7%), pine nut (12.2%) and peas and lentils (7.3%).
Lastly, the study outlined that three of the foods/food groups that had cases of the highest severity also had reports of being a hidden presence. These included buckwheat (16.9%), goat’s and sheep’s milk (15.5%) and peas and lentils (9%). Notably, pine nut was also found to be a hidden allergen in 4.1% of the pine nut-induced anaphylaxis cases.
“We are particularly emphasizing the case of anaphylaxis to goat and sheep milk,” Van der Brempt told Healio. “To date, our network has recorded a total of 97 cases, 13 more since the end of our work. These cases were studied in more detail and published very recently by Guillaume Pouessel, MD, from our group.
“Contrary to popular belief, while cow’s milk allergy is often associated with goat and sheep milk allergy, the reverse is rarely true: only 13% of our cases of anaphylaxis to goat and sheep milk had a history of cow’s milk allergy, most often cured,” Van der Brempt said. “This allergy is often severe and may be triggered by tiny amounts of goat and sheep milk, present as contaminants in milk-based products.”
Reflecting on the study, Van der Brempt said it showcases why allergy monitoring networks are important and useful.
“These networks are not yet available in all countries,” Van der Brempt told Healio. “Nearly 400 allergists collaborated on this work, thanks to their declarations, mainly in France, Belgium and Luxembourg. We hope that our work and others will in the future help to improve the quality of life of our food allergic patients.”
References:
For more information:
Xavier Van der Brempt, MD, PhD, can be reached at reseau@allergyvigilance.org.