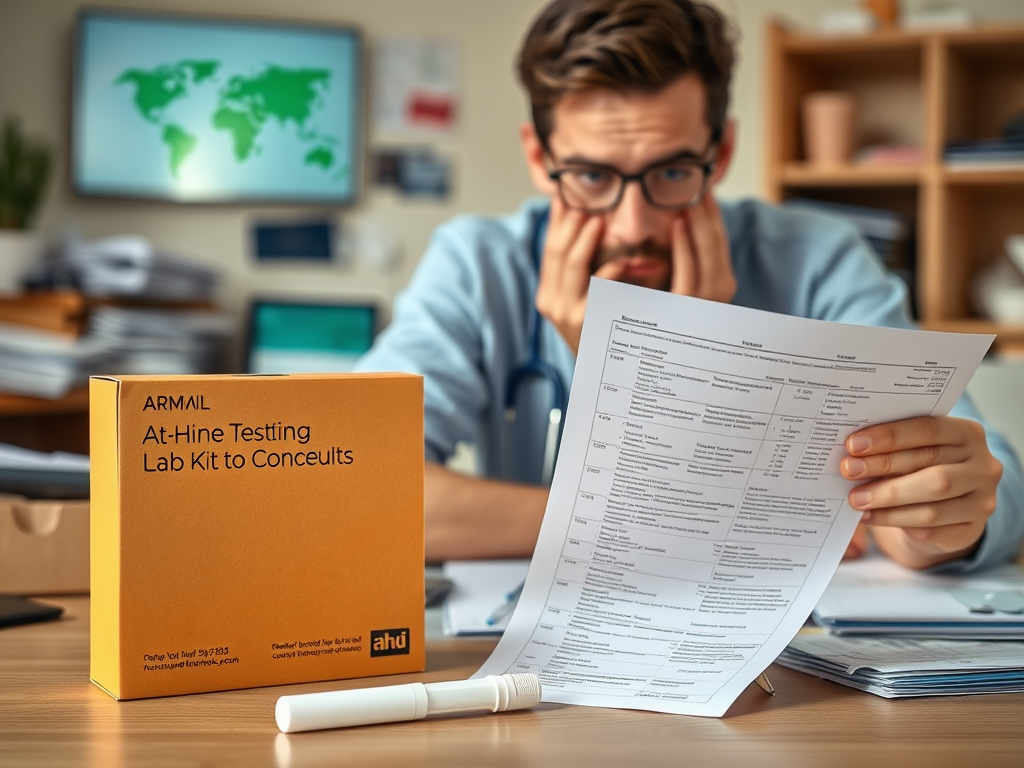
At-home lab and genetic tests are booming, and it’s easy to see why: people want convenience, privacy, and more control over their own health. The problem is that a medical test result without a physician’s context is just a number. This can easily lead to false alarms or confusing findings, which in turn cause a lot of unnecessary anxiety and follow-up procedures. This is especially true for genetic tests, which often turn up “variants of uncertain significance”—basically, genetic quirks that even scientists don’t fully understand. For someone at home, it’s easy to see that and assume the worst. This places physicians in a difficult position. They’re forced into a reactive role, trying to make sense of results they didn’t order, which can damage trust and make it harder to make decisions together.
When testing occurs in this piecemeal way, it creates a messy and confusing treatment path, leads to wasted money on repeated tests, and even increases the risk of medical errors.
So, the real issue isn’t that people have access to these tests. It’s that there’s no medical guidance on when to use them and what to do with the results.
More data doesn’t automatically lead to better health. Without proper interpretation, it can often do more harm than good.
Over the last decade, and especially since COVID made remote healthcare the norm, more and more of us have started ordering our own lab and genetic tests online, without ever talking to a doctor or dealing with insurance.
Want to check your cholesterol? Click.
Curious about your hormone levels? Click.
Worried about your risk for cancer, heart disease, or Alzheimer’s? A few more clicks and a kit is on its way.
The companies behind these tests market this as empowerment. They tell us to “own your data,” “take control of your health,” and cut out the “gatekeepers.” But in reality, bypassing doctors and the clinical context they provide creates a cascade of serious problems—not just for patients, but for the quality of care and the healthcare system as a whole. This isn’t just a new consumer trend; it’s a fundamental shift in how medical decisions get made, and all too often, how they go wrong.
And this trend is exploding. The direct-to-consumer genetic testing market is on track to be worth billions in the next decade, with millions of Americans already using services like 23andMe, Everlywell, and LetsGetChecked. Surveys show that a huge number of people either never discuss their results with a doctor or only do so after they’ve already decided what they mean. The key selling points are convenience, privacy, and autonomy. The hidden cost is complexity, misinterpretation, anxiety, and conflict.
The biggest issue is that a lab result on its own is practically meaningless. Medical tests aren’t a simple yes or no; they’re about probabilities. A number is just a number until it’s placed in the context of your symptoms, your medical and family history, your age, and other medications you’re taking. Without that clinical frame, people are left to connect the dots themselves, and they often draw the wrong picture.
For example, someone might order an inflammation panel, see an elevated C-reactive protein (CRP) level, and immediately conclude they have a serious autoimmune disease. They show up at a doctor’s office demanding powerful drugs, when in reality, the high CRP could just be from a minor cold or even obesity-related inflammation. Numbers without context create narratives, and those narratives are often flat-out wrong.
At home, laboratory and genetic testing are even more challenging. Most of what these tests find isn’t a clear-cut “you have this disease.” Instead, you get a lot of “variants of uncertain significance” (VUS)—basically, genetic quirks that scientists don’t yet understand. To a clinician, a VUS is usually just informational noise. But to a patient, it can sound terrifying. This uncertainty sends people spiraling. They end up in specialists’ offices, getting unnecessary scans and follow-up tests, or even asking for preventative surgeries based on a sliver of ambiguous data. This isn’t preventative care; it’s just fueling anxiety about diseases that will likely never happen.
This new dynamic is also putting doctors in an impossible position. More and more, patients aren’t coming in for a diagnosis; they’re arriving with a stack of self-ordered test results, a pre-formed conclusion about what’s wrong with them, and a specific treatment they want. The doctor’s role shifts from trusted diagnostician to a gatekeeper who has to say “no.” To the patient, this can feel dismissive, as if the doctor isn’t listening. The conversation changes from, “Doctor, can you help me figure out what’s going on?” to “Here are my results. Either confirm what I already believe or prove me wrong.” It’s turning medicine into an adversarial process and eroding the trust that holds the doctor-patient relationship together.
When testing is separated from actual medical care, the patient’s journey becomes dangerously fragmented. You might get a lab test from one company, a genetic analysis from another, and a “personalized” supplement plan from a third—all before ever talking to your own doctor, who is left trying to piece together a coherent story from incomplete information. This chaos leads to redundant tests, conflicting advice, and a higher risk of dangerous drug interactions.
These companies are selling us a consumer model for healthcare: more data is better, faster is better, and doing it yourself is best. But medicine isn’t like shopping on Amazon. In healthcare, more testing can lead to more false alarms. Faster decisions can lead to more mistakes. And autonomy without expertise is just a gamble. Healthcare is a high-stakes world of uncertainty, where careful interpretation is far more important than just having access to raw data. Insurance companies ultimately bear the cost of a cascade of unnecessary follow-ups, and clinicians burn out by spending their limited time refuting online theories instead of providing care.
At its heart, the problem isn’t the testing itself—it’s testing without guidance. Medicine has always been about managing uncertainty: knowing who to test, when to test, and, just as importantly, when not to act on a result. Direct-to-consumer testing undermines that entire framework. We’re left with a system where patients feel empowered but are often misinformed, and doctors are left to clean up the mess.
This trend appears to be progressing because it provides more data to us. But healthcare was never just a data problem; it’s an interpretation problem. By treating it like one, we trade real medical wisdom for a false sense of certainty, which only fuels anxiety, unnecessary treatments, and a breakdown of trust. The goal shouldn’t be to bypass doctors, but to find ways to bring better information into a stronger, more collaborative relationship with them. After all, a lab result is just data; a trusted doctor helps turn that data into wisdom.