January 08, 2026
3 min read
Key takeaways:
- VT-1953, a first-in-class topical immunomodulator, improved malodor associated with malignant fungating wounds in a phase 2 study.
- Participants also reported improved quality of life and wound pain reduction.
An investigational immunomodulator gel significantly improved malodor and measures related to pain and quality of life for people with malignant fungating wounds, according to findings from a phase 2 study.
In a press release, Vyome announced that VT-1953, a dual DNA gyrase and myeloid differentiation protein 2 (MD2) and toll-like receptor 4 (TL4) inhibitor, achieved its primary and secondary endpoints.

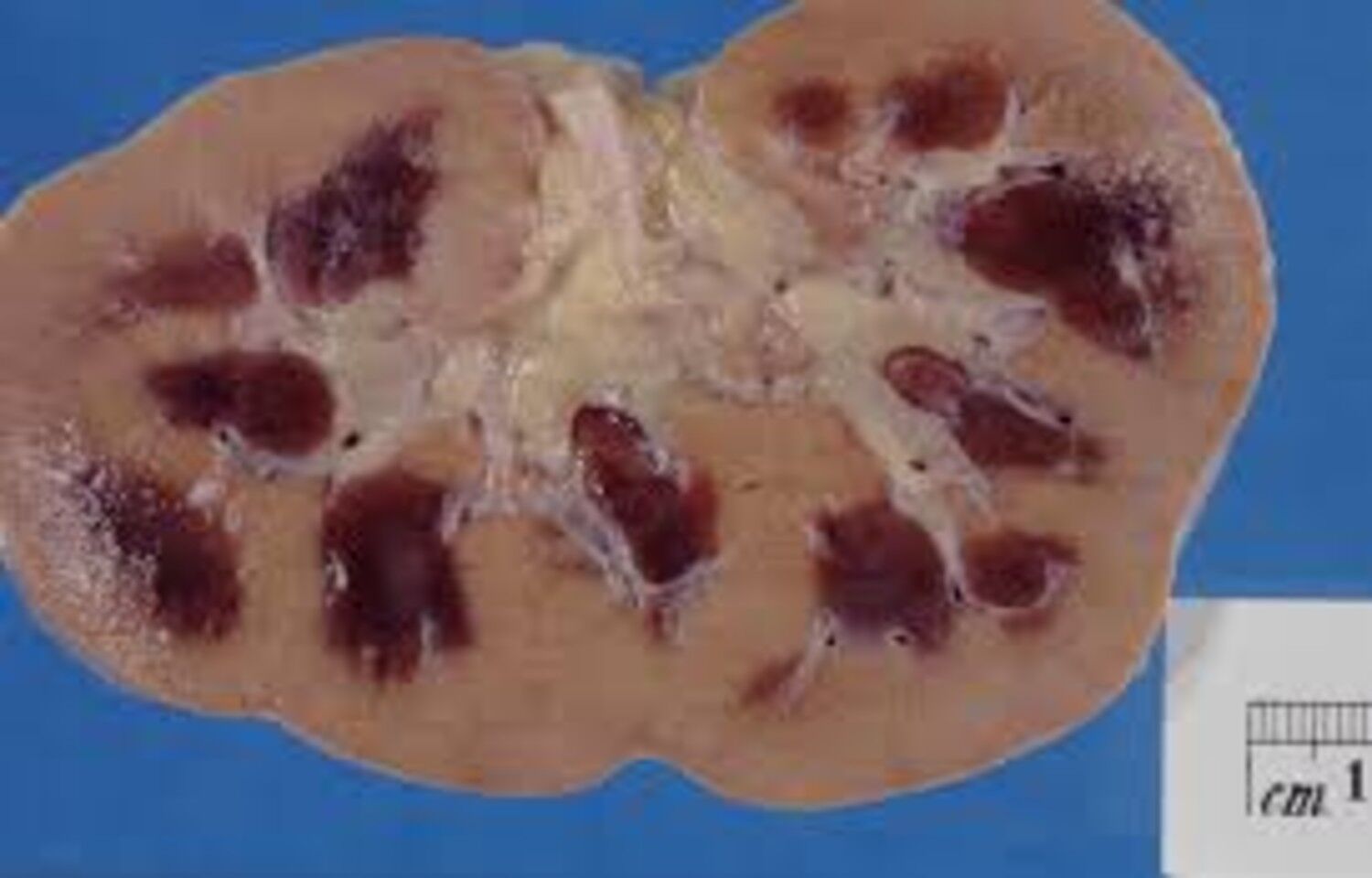
Approximately 5% to 15% of people with advanced cancers, particularly head and neck and breast cancers, can develop a malignant fungating wound, Aditya Bardia, MD, MPH, FASCO, professor of medicine and program director of breast medical oncology at UCLA Health Jonsson Comprehensive Cancer Center, told Healio.
“It is something that we see with disease progression,” Bardia said during an interview. “As the cancer progresses, it can invade the skin. When it invades the skin, that can result in the formation of a malignant fungating wound. This has a major impact on a patient’s quality of life, because malignant fungating wounds are typically associated with a malodor. That impacts not only impact the patient, but also the caregivers, and sometimes makes it difficult for the patients to participate in social activities or leave the house. It can be very distressing for the patient.”
There are no FDA-approved treatments for malignant fungating wounds, which are generally managed with supportive therapies such as dressing changes, topical gels, antibiotics and painkillers. In addition to malodor, patients with cancer-related wounds often report pain and itching caused by inflammation, Bardia said.
“This is a major unmet need in our field of oncology,” Bardia said. “The drug has a dual mechanism of action. It blocks DNA gyrase, and that can reduce or eliminate the bacteria that is associated with the production of malodor in these wounds. The second is that it can also reduce inflammation. It blocks the MD2-TLR4 interaction, reducing inflammation that is associated with these wounds.”
For the single-arm study, researchers assessed participants with malignant fungating wounds who received VT-1953, administered topically twice a day for 14 days. The primary endpoint was difference in the mean malodor score on day 14 compared with baseline. Exploratory endpoints included differences in mean pain scores and quality of life scores compared with baseline.
Researchers found that participants who received VT-1953 achieved a statistically significant improvement in odor at 14 days (P = .002). The improvement was significant at 14 days when compared with vehicle-treated participants (P = .0015), and researchers observed improvement as early as day 7 (P = .015).
“For some patients, you could detect the smell as far as 15 feet away,” Bardia said. “They received this drug for 14 days, and then the odor was assessed again. What we saw was a significant reduction in the malodor for most of the patients. Severe malodor was essentially gone, leaving only a mild smell.”
The drug was well-tolerated by participants, according to the release.
For the secondary endpoint of patient-reported impact of bad smell on the quality of life, participants who received VT-1953 saw a statistically significant improvement compared with vehicle-treatment by day 14 (P = .0256).
Additionally, 90% of participants reported a clinically significant two-point drop in pain score, Bardia said.
Treatment with VT-1953 was also associated with a significant improvement in quality-of-life component score by day 14 compared with baseline (P = .002) and with vehicle treatment (P = .0032).
Vyome CEO Venkat Nelabhotla said in the release that the company plans to design and initiate a pivotal phase 3 trial this year.
“If results are positive, that would potentially lead to approval of this drug,” Bardia told Healio. “This could become the first drug that is approved in the U.S. for patients with malignant fungating wounds.”
For more information:
Aditya Bardia, MD, MPH, FASCO, can be reached at abardia@mednet.ucla.edu.