January 08, 2026
3 min read
Key takeaways:
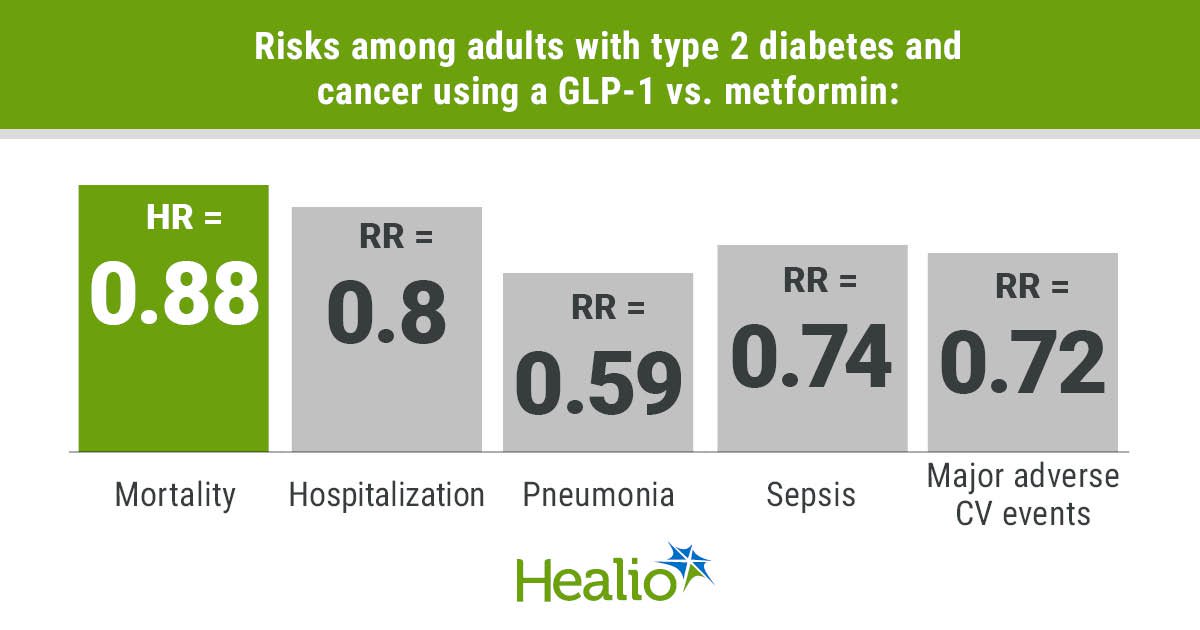
- Adults with type 2 diabetes and cancer had reduced risk for death if they used a GLP-1 vs. metformin.
- GLP-1s also conferred a lower risk for hospitalization, pneumonia, heart-related events and sepsis.
Adults with type 2 diabetes and cancer who used a GLP-1 had a lower risk for death and hospitalization compared with adults who used metformin, according to findings published in The Journal of Clinical Endocrinology & Metabolism.

Zoe Quandt
“Our findings build on prior reports of lower cancer rates in patients on GLP-1s, showing that patients that are prescribed GLP-1s have better survival than those without these agents, particularly in comparison to the addition of insulin,” Zoe Quandt, MD, MS, assistant professor in the division of diabetes, endocrinology and metabolism at the Diabetes Center at University of California, San Francisco, told Healio. “This suggests that we should consider the potential for these drugs to benefit patients in more ways than just the well-established metabolic and cardiac effects.”

Data were derived from Mahadevan A, et al. J Clin Endocrinol Metab. 2026;doi:10.1210/clinem/dgaf703.
Quandt and colleagues collected data from adults with type 2 diabetes who were diagnosed with a cancer that was ranked in the top 10 causes of cancer-related death for men and women. Propensity score matching was used to compare 3,551 adults who used a GLP-1 up to 3 months before or after systemic cancer therapy with 3,551 adults who used metformin. The group using GLP-1s included adults receiving liraglutide (Victoza, Novo Nordisk), dulaglutide (Trulicity, Eli Lilly), semaglutide (Ozempic, Novo Nordisk), exenatide and tirzepatide (Mounjaro, Eli Lilly).
Quandt said the number of adults with type 2 diabetes and cancer who were using GLP-1s in the study was noteworthy.
“Many endocrinologists and primary care providers are fearful of adding GLP-1s when patients are undergoing active therapy for cancer because of overlapping side effects,” Quandt said. “Our analysis suggests that many providers are willing to give it a try, even as monotherapy, with benefit to the patients.”
Adults who used a GLP-1 had lower risk for all-cause mortality than those using metformin (HR = 0.88; 95% CI, 0.78-0.99; P = .0368). The GLP-1 group also had lower risk for all-cause hospitalization (RR = 0.8; 95% CI, 0.74-0.86; P = .0004), pneumonia (RR = 0.59; 95% CI, 0.48-0.72; P = .0004), sepsis (RR = 0.74; 95% CI, 0.61-0.89; P = .004), major adverse cardiovascular events (RR = 0.72; 95% CI, 0.58-0.9; P = .0053) and pulmonary embolism (RR = 0.61; 95% CI, 0.44-0.84; P = .004) than adults using metformin. There was no difference in risk for diabetic ketoacidosis or hyperosmolar hyperglycemic state between the groups.

Aditya Mahadevan
“Metformin is a standard, first-line antihyperglycemic and I would expect that patients in this cohort had better diabetes control,” Aditya Mahadevan, MD, resident physician in the department of medicine at University of California, San Francisco, told Healio. “In that sense, it surprised me that patients on GLP-1 monotherapy outperformed [metformin] in terms of survival and hospitalization outcomes. Additionally, metformin has been shown to be well-tolerated in patients with active cancer, making our outcomes more meaningful by comparison.”
In a subanalysis, researchers matched 1,620 adults with type 2 diabetes on metformin who were newly starting a GLP-1 with those on metformin who were newly starting insulin up to 3 months before or after initiating systemic cancer therapy. Adults starting a GLP-1 had lower all-cause mortality risk than those initiating insulin (HR = 0.79; 95% CI, 0.66-0.93; P = .0062).
“I think the beneficial outcomes in patients who received metformin and were newly started on a GLP-1 suggest that there could be synergy between these two in patients with diabetes and cancer,” Mahadevan said.
Based on the study’s findings, Mahadevan said, prospective studies are needed to see if the findings are similar in real-world cohorts.
“In particular, I would like to see clinical outcomes in patients with obesity started on GLP-1 receptor agonists while receiving cancer treatment,” Mahadevan said. “Additionally, I would like to see further preclinical and prospective studies that could explain or validate the association between GLP-1 usage and reduced rates of pulmonary embolism, as this stood out as a huge potential benefit in patients with cancer.”
For more information:
Aditya Mahadevan, MD, can be reached at aditya.mahadevan@ucsf.edu.
Zoe Quandt, MD, MS, can be reached at zoe.quandt@ucsf.edu.