[ad_1]
January 07, 2026
4 min read
Key takeaways:
- The chronic stress that follows adverse childhood experiences may lead to maladaptive behavior.
- Adaptive coping may reduce risks for negative outcomes in physical and mental health.
DALLAS — Sleep and satisfaction with social support mediated the relationship between adverse childhood experiences and depressive symptoms, according to data presented at the American College of Lifestyle Medicine’s annual meeting.
But stress, substance use, diet, quantity of social support and physical activity did not significantly impact this relationship, Liana Abascal, PhD, MPH, DipACLM, associate professor, California School of Professional Psychology at Alliant International University, said during her presentation.

Data derived from Mraz A, et al. The influence of lifestyle medicine on the relationship between adverse childhood experiences, depressive symptoms, and suicidal ideation. Presented at Lifestyle Medicine 2025; Nov. 16-19, 2025; Dallas.
“It’s a real simple measure,” Abascal said. “Did any of these 10 things happen to you, or were they in your environment?”
Adverse childhood experiences (ACEs) include emotional, physical or sexual abuse as well as emotional or physical neglect. Living with someone experiencing substance misuse, mental illness, suicidal thoughts and behavior, divorce or separation, incarceration, or intimate partner or domestic violence also qualifies as an ACE.
“As ACEs go up, we see worse mental health and worse physical health, and it’s pretty dramatic,” Abascal said. “But we don’t know a lot about the mechanisms of effect.”

Liana Abascal
Patients with chronic stress may develop maladaptive behavior that leads to disease, disability and social problems, she noted, yet adaptive coping may reduce the risks for negative mental health outcomes.
“It suggests a possible relationship,” Abascal said.
The cross-sectional, quantitative study included 115 adults (74% women; predominantly white) aged 18 to 77 years (mean age, 32 years) recruited from Reddit and other social media platforms as well as via word-of-mouth snowball sampling for participants who then completed the ACEs Questionnaire.
“Our average number of ACEs was about 2.5, even though we did see the full range of ACEs from 0 to 10,” Abascal said.
Participants also completed questionnaires evaluating the “six pillars” of diet, physical activity, sleep quality, stress management, substance use and quantity of and satisfaction with social support.
“Do these six pillars mediate the relationship between ACEs and depressive symptoms?” Abascal said.
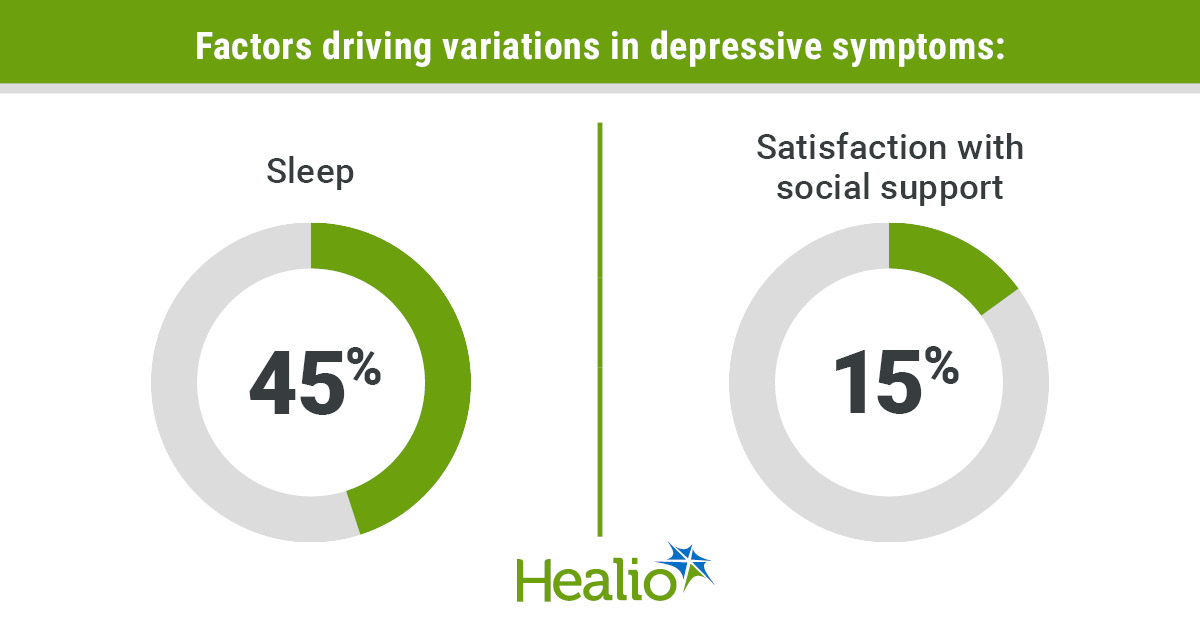
Sleep as measured by the Pittsburgh Sleep Quality Index was a significant mediator of Patient Health Questionnaire-9 (PHQ-9) scores, Abascal said, and ACEs had an indirect effect on PHQ-9 scores as well (95% CI, 0.128-0.784). Additionally, sleep accounted for 45% of the variation in depressive symptoms.
Specifically, sleep was significant for women and participants with medium socioeconomic status as well as for participants who did not identify as Hispanic, Latino or of Spanish origin and for those who did identify as white.
“That really was predominantly our sample, anyway, so that’s not surprising,” Abascal said.
Satisfaction with social support also was a significant mediator between PHQ-9 scores and ACEs, Abascal continued, noting that ACEs had an indirect effect on PHQ-9 (95% CI, 0.001-0.308). This satisfaction accounted for 15% of the variation in depressive symptoms as well.
Abascal noted previous research indicating a relationship between social support and depressive symptoms, adding that this support may buffer relationships between ACEs and adult mental health.
While the quality of social support had a significant effect on the relationship between ACEs and depression, the quantity of social support did not, nor did stress, substance use, diet or physical activity.
“It was interesting that the quality was significant and not the amount,” Abascal said.
Abascal attributed the lack of impact among these pillars to their complexity, the self-reported nature of the data and the potential presence of other mediating mechanisms that were not included in this study.
Similarly, none of the six pillars that Abascal described were significant mediators in the relationship between ACEs and suicidal ideation (SI). Gender identity, cultural background, and socioeconomic status did not have any significant impact on this relationship either.
“Why didn’t we see an effect with suicidal ideation? It’s a tricky one. There’s a lot of things that go into SI,” Abascal said.
Influences on SI may extend beyond lifestyle coping behaviors and include hopelessness, acquired capability, perceived burdensomeness and thwarted belonginess, she said. Participants also may underreport SI because of discomfort, fear of judgment or the stigma associated with it.
“If someone is suicidal and they don’t want help, they will not endorse being suicidal,” Abascal said.
These findings highlight the importance of sleep as well as assessing and treating sleep problems, she continued.
“We have great treatments for sleep,” she said.
Abascal cited psychoeducation and cognitive behavioral therapy for sleep insomnia, such as the CBT-i Coach free mobile app developed by the U.S. Department of Veterans Affairs, in addition to medications as a last resort.
“Sleep is the foundation of coping,” she said. “If you haven’t slept, certainly, it makes it a lot harder to make some positive decisions and engage in healthful behavior.”
Abascal also emphasized the importance of discussing social support with patients.
“That’s something that really does not happen, I think, a lot within the medical world,” she said. “Hopefully, psychology is doing a little bit better with that.”
Recommendations include referrals for specific social support groups, prosocial community activities, family therapy when indicated and respite for caregivers.
Looking ahead, Abascal said that longitudinal research using multiple measures for each of these constructs and/or observational data along with purposive sampling for greater variety in the population would provide more confidence for these conclusions.
“And it would be interesting, of course, to look at other coping behavior that is outside of what we see in the health behaviors,” Abascal said.
For more information:
Liana Abascal, PhD, MPH, DipACLM, can be reached at psychiatry@healio.com.
[ad_2]
Source link