One of the main barometers I use to rapidly characterize an ED as either a resuscitation shop or a standard (read resuscitation sub-standard) ED is are they placing arterial lines.
I have covered all things a-lines in the past:
Today’s show will be a little different. It is a response to comments made on the EM:RAP show in June 2024. I also was sparked to discuss this by a tweet about the show, the PITT, in which an ICU doc said the show was unrealistic b/c they had never been in an ED in which arterial lines were placed.
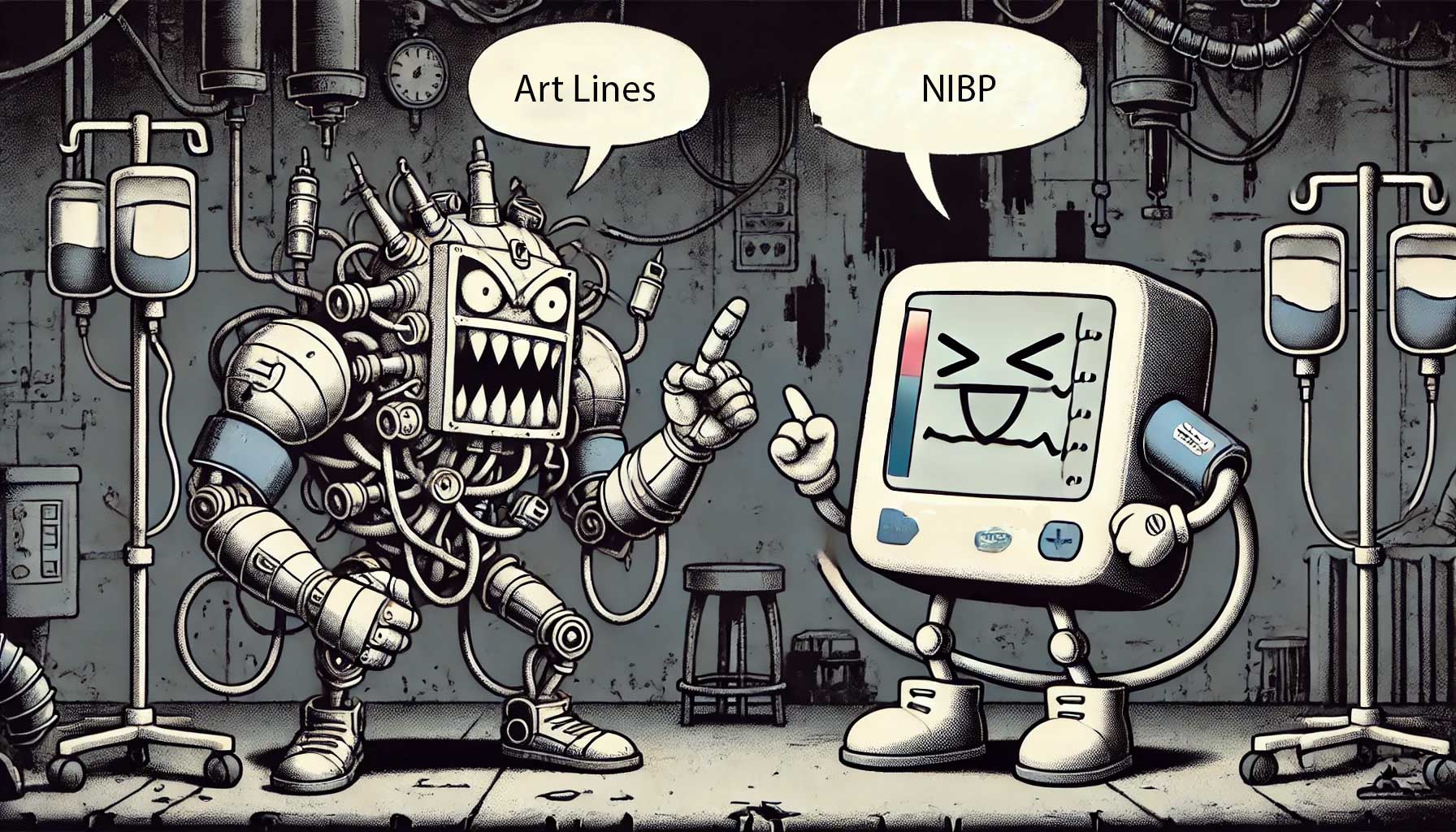
Necessity Of Arterial Lines
Accuracy
When NIBP Cuffs are Inaccurate
All three- SBP, MAP, and DBP are all measured
Bradycardia only an issue < 40 BPM
Skinny or fat is not an issue unless pt doesn’t have the right cuff
Biggest issue is malperfused states or shock, especially with profound peripheral vasoconstriction. Hemorrhagic shock makes a-lines a necessity, with a femoral placement.
Cuff timing q 30 minutes
New Study
Perera et al. Non-invasive versus arterial pressure monitoring in the pre-hospital critical care environment: a paired comparison of concurrently recorded measurements
Prehospital Environment, >2000 paired observations of NIBP and Arterial Line
Bounds of agreement: <20 mmHg for systolic BP (SBP) and diastolic BP (DBP) and <10 mmHg
Only 64% of SBP, 76% of DBP, and 55% of MAP measurements fell within the pre-defined acceptable ranges. NIBP readings tended to overestimate SBP and MAP at low BP values (hypotension) and underestimate these values at high BP values (hypertension). DBP was consistently overestimated across its range.
- Impact of Hemodynamic Instability: Hemodynamic shock was associated with lower agreement for SBP (adjusted odds ratio [aOR] 0.52), DBP (aOR 0.65), and MAP (aOR 0.53).
- Impact of Severe Hypertension: Severe hypertension was associated with markedly reduced agreement for SBP (aOR 0.17), while DBP and MAP were less affected.
- Impact of Arterial Catheter Site: Femoral arterial lines were associated with reduced agreement for MAP (aOR 0.65) compared to radial lines, .
- from St Emlyns’ Post
Ability to Real-Time Monitor
It is usually during the resuscitative period, not long-term that a-lines really shine–I still want them long term, obviously.
Opportunity Cost
Nursing
Should already be 1:2 nursing
What about: We have ED nurses, not ICU nurses; they are not trained on how to set-up arterial lines.
See this video for how to set-up a pressure transducer
Docs
Time to Place A-lines
London HEMs experience is 2 minutes. Only get that way if you are good, but this is a transferable skill from ultrasound-guided intravenous lines
Parker Labs Ultradrape & Ultradrape II
Indication Creep
There never would need to be an indication restriction, so there can’t be indication creep
ICU Expectations
This is the one I hear most commonly–I think it is a straw man.
The one that truly galls me is, “If we allow arterial lines, the ICU won’t feel the same urgency to get them upstairs!” So if we provide crappy care, the intensivists will doubt our capability of caring for sick patients and rush to get them to a safe place. That is not how I want Emergency Medicine thought of.
Additional New Information
More on EMCrit
Additional Resources
You Need an EMCrit Membership to see this content. Login here if you already have one.