October 08, 2025
2 min read
Key takeaways:
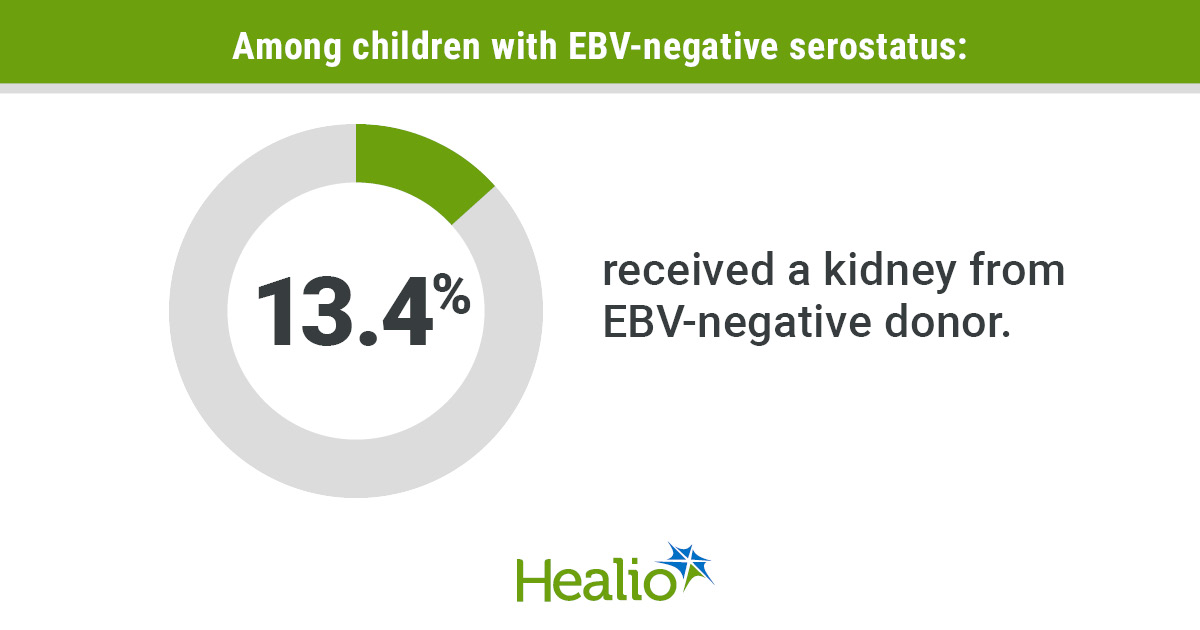
- Less than 14% of EBV-negative children received a kidney from an EBV-negative donor.
- Many EBV-negative kidneys went to EBV-positive adults.
- Accounting for EBV serostatus in organ allocation systems could help.
Children negative for Epstein-Barr virus, or EBV, undergoing kidney transplant often received EBV-positive kidneys despite the risk this poses and the availability of EBV-negative donor kidneys, according to study results published in JAMA.
Previous research has shown risk for posttransplant lymphoproliferative disorder, a type of cancer, is highest when EBV-seronegative recipients received kidneys from EBV-seropositive donors, with children especially at risk, according to Vishnu S. Potluri, MD, MPH, assistant professor of medicine at the Hospital of the University of Pennsylvania, Sandra Amaral, MD, MHS, associate professor of pediatrics and epidemiology at the University of Pennsylvania and medical director of the pediatric transplant program at the Children’s Hospital of Philadelphia, and colleagues.

Data derived from Potluri VS, et al. JAMA. 2025;doi:10.1001/jama.2025.14067.
Understanding the risks to children in need of kidney transplants is needed to effectively optimize transplant allocation and reduce risks for infection and malignancy, according to Potluri and Amaral.

Vishnu S. Potluri
“Children are some of our most vulnerable patients, and they have the greatest opportunity at having a meaningful life if the allocation system continues to help get them high-quality organs,” Potluri told Healio.
Using 2018 to 2023 data from the Organ Procurement and Transplantation Network, the researchers ascertained the EBV serostatus of child and adult kidney recipients.
In total, they reviewed kidneys from 61,368 donors, of which 40.1% had a kidney donor profile index score less than 35%, a marker of better organ quality.
Further, 4,730 kidneys from 2,421 donors (9.8%; median age, 22 years; 74.2% male, 79.8% white) were EBV seronegative, with 1,071 donors (44.2%) having both EBV-negative serostatus and ideal pediatric-quality kidneys. There were 43,275 EBV-seropositive kidneys from 22,218 donors (90.1%; median age, 29 years; 69.3% male; 67% white).
Among 3,300 children who underwent kidney transplants, 42% (n = 1,399) were EBV negative, yet only 13.4% received a kidney from an EBV-negative donor (n = 188). Many EBV-negative kidneys went to EBV-positive adults (n = 3,778).

Sandra Amaral
“I was very disappointed to see so many organs that were EBV negative allocated to recipients who really don’t benefit as much from that particular donor characteristic,” Amaral told Healio. “I was struck by the untapped opportunity to allocate these organs to children, which could really confer increased protection.”
Overall, the researchers suggest that accounting for EBV serostatus in organ allocation systems could be a helpful modification.
“What we really need is a relatively minor and modest change to the allocation system, which could have a big impact for a small group of very vulnerable patients,” Potluri said.
Amaral said the use of more weighted models could be a way to initiate change without “upending” the current system.
“If we weighted certain factors differently instead of getting points for a specific category, we could get composite scores that could provide more protection with very little impact to the overall allocation of organs,” she said. “It’s another move toward precision medicine and optimizing the safety and efficacy of the appropriate organ for the appropriate recipient.”
Potluri and Amaral agreed that shared decision-making is key to keeping the organ allocation system successful, including collaboration between pediatric and adult nephrologists.
“It requires a multiteam effort and lots of advocacy,” Potluri said.
For more information:
Sandra Amaral, MD, MHS, can be reached at amarals@chop.edu.
Vishnu S. Potluri, MD, MPH, can be reached at vishnu.potluri@pennmedicine.upenn.edu.