September 08, 2025
7 min read
A 68-year-old man presented to an outside emergency department with 2 days of progressive bilateral eyelid swelling.
He had a history of stage IVa transglottic laryngeal squamous cell carcinoma status post laryngectomy, bilateral neck dissection, and adjuvant chemoradiation currently on pembrolizumab complicated by immune checkpoint inhibitor-associated truncal and facial rash on prednisone.

Source: James T. Kwan, MD, and Victoria S. North, MD
His ocular history was notable for cataract extraction with IOL implantation in both eyes several years prior. His social history included a 20-pack-year cigarette smoking history.
Examination and workup
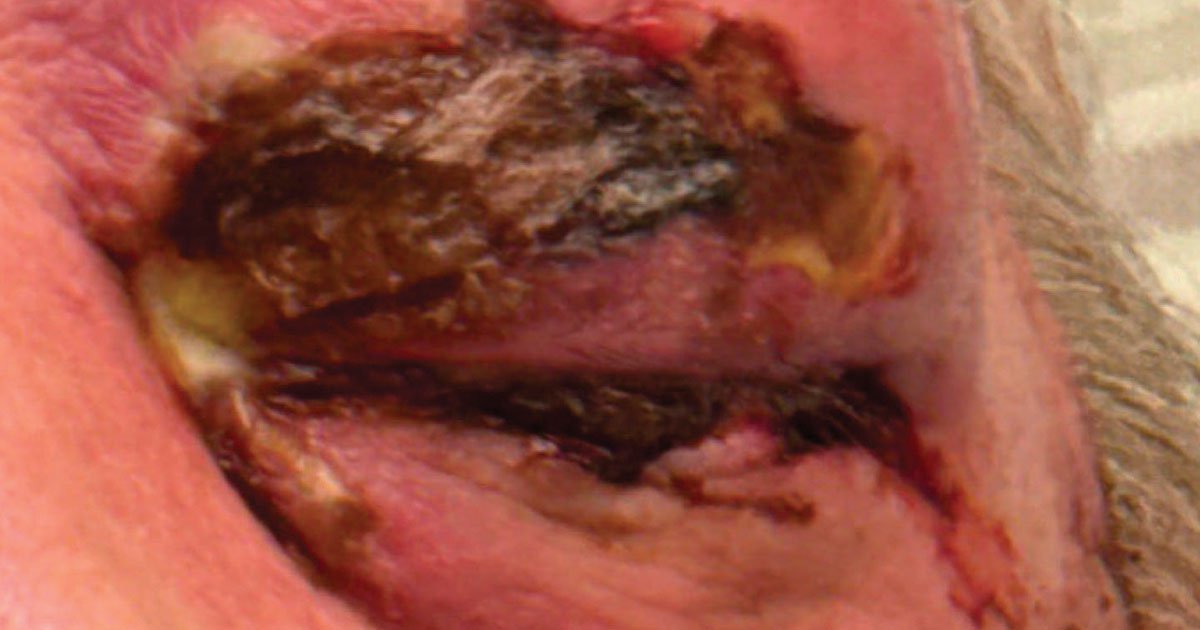
On presentation, the patient was hemodynamically stable with blood pressure 126/84 mm Hg, pulse 110 beats per minute, temperature 98.4°F, respiratory rate 16 breaths per minute and oxygen saturation 96%. Visual acuity was 20/200 in the right eye and hand motion in the left eye. IOP was 20 mm Hg in the right eye and 27 mm Hg in the left eye. The right pupil was normal, and the left pupil was fixed and mid-dilated with an afferent pupillary defect by reverse. Extraocular movements were limited in all gaze directions in the right eye with complete ophthalmoplegia in the left eye. External examination demonstrated bilateral upper and lower eyelid erythema and tense edema with overlying areas of purulence and eschar formation (Figure 1). Anterior examination was notable for 2+ diffuse conjunctival injection in the right eye and 360° severe injection in the left eye with subconjunctival hemorrhage and purulent discharge. Posterior segment examination was limited but notable for only a single cotton wool spot in the right eye.
An urgent CT maxillofacial was performed, demonstrating hypoattenuated collections within the right and left upper eyelids with possible extension into the anterior orbit on the left (Figure 2).

A comprehensive metabolic panel was notable for hyponatremia (126 mEq/L) with an anion gap of 17 mEq/L, elevated creatinine (1.01 mg/dL) and hyperglycemia (168 mg/dL). Complete blood count with differential was within normal range: white blood cell count 11.4 K/µL, hemoglobin 13.3 g/dL and platelets 324 K/µL. Lactate was significantly elevated at 5 mmol/L.
What is your diagnosis?
See answer below.
Tissue necrosis, significant purulence
Given the extensive periorbital swelling and erythema, evidence of optic nerve compromise on examination (decreased vision, relative afferent pupillary defect, complete ophthalmoplegia), and extension of the hypoattenuating collections into the orbit on CT maxillofacial, a diagnosis of orbital cellulitis was made. More concerning was the presence of tissue necrosis and significant purulence, which suggested periorbital necrotizing fasciitis.
Next steps
The patient was immediately started on broad-spectrum IV antibiotics including vancomycin, ceftazidime and metronidazole, in addition to topical moxifloxacin eye drops. Given concern for optic nerve compromise, the outside emergency department performed a left-sided lateral canthotomy and cantholysis. After the procedure, visual acuity improved to 20/400 in the left eye, and the pupil became slightly more reactive. Purulent material was expressed and sent for Gram stain and culture. At that time, it was determined that the patient required a higher level of specialty care, and a transfer to Tufts Medical Center was initiated. En route, the patient became acutely hypotensive and was given 3 L of IV crystalloid.


Upon the patient’s arrival, lactate had improved to 3.3 mmol/L. Broad-spectrum antibiotics were continued, and IV clindamycin was added for antitoxin effect. Repeat ophthalmologic exam was largely unchanged, with the exception of increased dark eschar formation overlying the left upper eyelid. Telemetry monitoring demonstrated runs of supraventricular tachycardia, and an electrocardiogram identified an inferior non-ST-elevation myocardial infarction. He underwent emergent cardiac catheterization with placement of a right coronary artery drug-eluting stent.

As soon as catheterization was complete, the ophthalmology team performed bedside debridement of the bilateral upper and lower eyelids as the patient was not stable enough to undergo general anesthesia. Necrotic tissue and purulent material were debrided until bleeding tissue was encountered (Figure 3). Tissue samples were sent for culture and pathologic evaluation. Wet-to-dry dressings soaked in dilute hypochlorous acid were applied to the eyelids. Subsequent MRI of the orbits showed a left periorbital abscess, and he underwent bedside incision and drainage with repeat debridement the following day. No deeper orbital extension of the necrotizing fasciitis or collection was noted.

Discussion
Our patient presented with bilateral periorbital necrotizing fasciitis, an ophthalmic emergency associated with high mortality rates, especially if there is any delay of care. Necrotizing fasciitis is a subset of the broader class of necrotizing soft tissue infections (NSTIs), including rapid soft tissue destruction of the skin, subcutaneous fat and muscle. NSTIs can be categorized as polymicrobial (type I) or monomicrobial (type II). Type II infections occur more commonly in immunocompetent patients (Hakkarainen et al.). The most commonly identified organism, especially for type II NSTIs, is Streptococcus pyogenes; however, Staphylococcus aureus, Enterococcus and Escherichia coli are also typical agents (McDermott et al.). In rare cases of NSTIs secondary to aquatic exposure, Vibrio vulnificus should be considered (Chang et al.). While the majority of NSTIs affect the limbs, about 2% to 10% of cases involve the head and neck, and orbit involvement can be life- and vision-threatening (McDermott et al.). A review of the literature by Amrith and colleagues indicates that of 95 cases of periorbital necrotizing fasciitis, approximately 8.5% of patients died, 14% experienced significant vision loss from central retinal artery occlusions or exenterations, and 7% required an exenteration.
The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score is a tool used to assist in detection of necrotizing fasciitis based on laboratory values, including C-reactive protein, white blood cell count, hemoglobin, sodium, creatinine and glucose levels. A score of less than 6 is considered low risk; however, when high clinical suspicion persists, immediate tissue debridement should be pursued regardless of the LRINEC score.
Surgical debridement
When periorbital necrotizing fasciitis is suspected, emergent debridement — whether at bedside or in the operating room — is crucial. Time is of the essence for these critically ill patients. These aggressive infections spread rapidly as the causative bacteria induce toxin-mediated inflammation, which leads to vascular thrombosis and subsequent tissue necrosis and enables unsuppressed microbial proliferation. Additionally, the bacterial toxins and host inflammatory response can lead to septic shock and potentially fatal end-organ damage (Angus et al.). Early debridement (within 12 hours) is associated with improved mortality rates as prompt action reduces the bacterial load and toxin exposure (Gelbard et al.). Debridement down to bleeding tissue is important to allow adequate delivery of systemic antibiotics and healing factors to the site of infection. Management should not be delayed in lieu of availability of a subspecialized surgeon. In addition, as the diagnosis of NSTIs can be made with clinical evaluation alone, confirmatory radiographic evidence is not necessary. Furthermore, while the presence of gas on radiographic evaluation is classic, only 24.8% of patients will have this finding at the time of presentation (McDermott et al.). Frequent reevaluation and re-debridement should be pursued when there is clinical or radiographic evidence of residual infection.
Antibiotics and other therapeutics
Prompt initiation of broad-spectrum IV antibiotics, with coverage of gram-positive, gram-negative and anaerobic organisms, is key. Coverage for MRSA at onset is indicated and can be adjusted when culture data and sensitivities become available. Clindamycin directly suppresses bacterial exotoxin production and should be added, although it is bacteriostatic and should not be used as monotherapy for these infections (Urbina et al.).
Hyperbaric oxygen is another tool that may reduce morbidity associated with the vascular thrombosis caused by NSTIs. While its safety has been demonstrated, data regarding impact on mortality are limited, and other steps in management should not be delayed in favor of hyperbaric oxygen (Lazzeri et al.).
Dilute hypochlorous acid is another promising therapy in periorbital necrotizing fasciitis management. First used for management of NSTIs of the limbs, unpublished data from Vanderbilt Eye Institute, presented at the American Society of Ophthalmic Plastic and Reconstructive Surgery 2024 Fall Scientific Symposium, demonstrated that use of dilute hypochlorous acid reduced rates of exenteration and mortality to 0 in a preliminary study of 17 orbits of 14 patients with periorbital necrotizing fasciitis (Crew et al.; Siktberg et al.). The authors propose that topical application of hypochlorous acid aids in neutralizing exotoxin directly at the source of infection, thereby leading to improved outcomes.
Case continued
The patient required intensive care for an additional week for hemodynamic instability and IV antibiotics. The dilute hypochlorous acid dressings were changed four times daily. Wound cultures grew 4+ Streptococcus pyogenes sensitive to penicillin, and the antimicrobial regimen was adjusted accordingly. No additional surgical debridement was required. Significant left upper and lower eyelid retraction occurred with wound healing, leading to chemosis and exposure keratitis. Bilayer Tegaderm (3M) moisture chambers with artificial tear ointment were applied to protect the ocular surface until a temporary tarsorrhaphy was performed. Significant improvement in exposure keratopathy and chemosis followed. He was discharged on oral cefadroxil and with close follow-up scheduled locally.
The patient was readmitted to Tufts Medical Center 3 weeks later for increased generalized malaise and concern for purulent discharge of the left eye. He reported an episode of eye rubbing several days prior that caused the temporary tarsorrhaphy to break. A repeat temporary tarsorrhaphy was performed (Figure 4), corneal cultures were sent, and topical antibiotics and aggressive ocular surface lubrication were reinitiated. The cultures were negative. A permanent tarsorrhaphy was discussed in depth with the patient, but he declined. He was discharged after a 10-day stay with local follow-up again arranged.

Since discharge, he underwent eyelid reconstruction with a local oculoplastics surgeon: bilateral lower eyelid cicatricial entropion repair via lateral tarsal strip and application of full-thickness skin grafts to the right lower and left upper eyelids. Per report, he is currently doing well.
Editor’s note: Consent was given from the patient in this article for publication.
- References:
- Amrith S, et al. Acta Ophthalmol. 2013;doi:10.1111/j.1755-3768.2012.02420.x.
- Angus DC, et al. N Engl J Med. 2013;doi:10.1056/NEJMra1208623.
- Chang CY, et al. World J Emerg Surg. 2022;doi:10.1186/s13017-022-00433-z.
- Crew JR, et al. Wounds. 2016;28(2):40-47.
- Gelbard RB, et al. J Trauma Acute Care Surg. 2018;doi:10.1097/TA.0000000000001857.
- Hakkarainen TW, et al. Curr Probl Surg. 2014;doi:10.1067/j.cpsurg.2014.06.001.
- Lazzeri D, et al. Ophthalmic Plast Reconstr Surg. 2010;doi:10.1097/IOP.0b013e3181e26821.
- McDermott J, et al. JAMA Surg. 2024;doi:10.1001/jamasurg.2024.3365.
- Siktberg J, et al. The use of dilute hypochlorous acid in the treatment of periorbital necrotizing fasciitis. Presented at: American Society of Ophthalmic Plastic and Reconstructive Surgery Fall Scientific Symposium; Oct. 17-18, 2024; Chicago.
- Urbina T, et al. Antibiotics (Basel). 2021;doi:10.3390/antibiotics10091104.
- For more information:
- Victoria S. North, MD, of New England Eye Center, Tufts University School of Medicine, can be reached at victoria.north@tuftsmedicine.org.
- Edited by Heba Mahjoub, MD, and James T. Kwan, MD, of New England Eye Center, Tufts University School of Medicine. They can be reached at james.kwan.ophthalmology@gmail.com and hmahjoub@tuftsmedicalcenter.org.