August 13, 2025
5 min read
Key takeaways:
- Patients with GI cancer who do not identify as white, have advanced disease or had recent treatment may have worse financial toxicity.
- Financial toxicity was associated with reduced medication use due to cost.
The most “vulnerable” individuals with gastrointestinal cancer can also experience the worst financial toxicity.
In a study of more than 8,000 patients, greater than 40% experienced financial toxicity and close to 30% reported at least one health-related social risk, including issues with food, housing or transportation.

Data derived from Narayan A, et al. JCO Oncol Pract. 2025;doi:10.1200/OP-25-00218.
Race, advanced disease and recent treatments all had significant associations with both.
Worse financial toxicity also had significant associations with reduced quality of life and medication adherence.

Kaitlyn Lapen
“They’re just already so vulnerable,” Kaitlyn Lapen, MD, a radiation oncology resident in her last year of training at Memorial Sloan Kettering Cancer Center, told Healio about these groups of patients.
“It’s disheartening.”
Prevalence, risk factors
Multiple studies have shown increased costs can significantly impact cancer care.
Healio previously reported that individuals with cancer who had high-deductible insurance plans experienced both shorter OS and cancer-specific survival.
Earlier this year, ASCO made multiple recommendations to stakeholders and Congress to reduce out-of-pocket expenses patients face.
“Many patients, especially those on public insurance programs such as Medicaid, struggle to afford additional medical expenses on top of essential goods such as food and shelter,” an ASCO position approved by the society’s board of directors in December reads. “According to one estimate, the average total cost of medical care and pharmaceuticals exceeds $42,000 in the year following a cancer diagnosis.”
Individuals with gastrointestinal malignancies may experience worse financial hardships because of the complex and multimodal therapies needed for treatment, according to study background.
Lapen and colleagues evaluated the prevalence of financial toxicity and health-related social risks, as well as predictors for both, in that patient population.
They used the Comprehensive Score for Financial Toxicity (COST) and patient-reported outcomes to investigate.
Researchers sent the standard institutional assessment to more than 70,000 patients between June 2022 and August 2023.
They included 8,335 individuals (49% aged 65 years and older; 53% men; 76% white) with gastrointestinal cancer in the study.
COST scores of 0 to 13 indicated severe financial toxicity and 14 to 25 moderate. Scores can reach 44.
Researchers assessed health-related social risks with the question, “Is the amount of income you have available in a typical month not enough for any of the following needs?” — food, housing, transportation, clothing, medications and repairs to home.
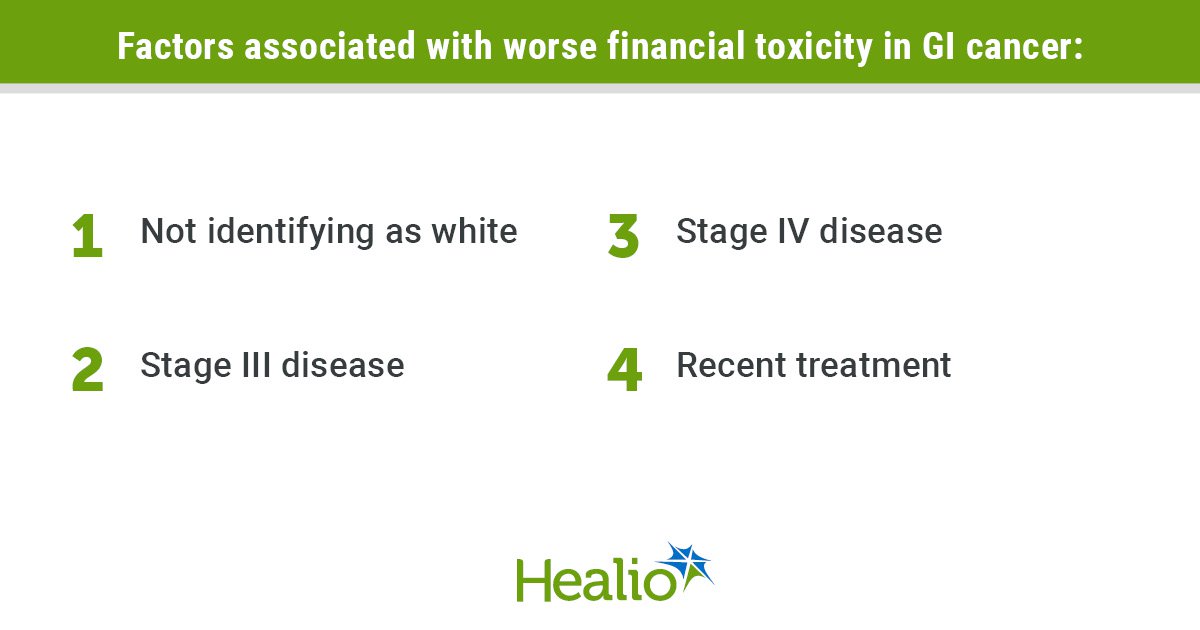
Factors associated with financial toxicity
The study population had a mean COST score of 24.3 (standard deviation, 10.7).
In all, 45% had financial toxicity, including 14% with a severe designation, and 28% reported experiencing at least one health-related social risk.
Additionally, 26% reported using some savings to pay for treatment, 3% used all their savings and 7% had no savings to start with.
Factors associated with financial toxicity included not identifying as white (B = 4.2; 95% CI, 3.61-4.78), having stage III (B = 1.33; 95% CI, 0.58-2.07) or stage IV disease (B = 1.56; 95% CI, 0.8-2.32), receiving a recent treatment (B = 3.23; 95% CI, 2.72-3.75), or having anal (B = 1.97; 95% CI, 0.66-3.29), esophageal (B = 1.66; 95% CI, 0.49-2.82) or hepatobiliary cancers (B = 1.05; 95% CI, 0.09-2).
Factors associated with at least one health-related social risk included not identifying as white (OR = 2.14; 95% CI, 1.9-2.4), having stage III (OR = 1.31; 95% CI, 1.12-1.54) or stage IV disease (OR = 1.24; 95% CI, 1.05-1.46), receiving a recent treatment (OR = 1.2; 95% CI, 1.08-1.34) or having gastric cancer (OR = 1.25; 95% CI, 1.02-1.52).
“Patients with more advanced disease are probably coming for more appointments,” Lapen said. “They’re likely coming for more evaluations and procedures, and likely using some long-term systemic therapy. There’s a shift in cancer; metastatic disease can be seen as a chronic disease requiring lifelong treatment — the more advanced the disease is, the more cumulative financial burden there is. It’s reflecting what we see with other chronic diseases.”
Financial toxicity had associations with using more savings to pay for care, taking fewer drugs because of costs and lower quality of life (all P < .001).
Factors associated with protectivity against financial toxicity and health-related social risks included being aged 65 years and older, having annual income of more than $100,000 and private insurance (all P < .001).
Researchers acknowledged study limitations, including being unable to determine causal relationships.
‘Screening into action’
Screening for financial toxicity has improved over the last several years.
Lapen and colleagues noted a National Comprehensive Cancer Network survey that found 76% of centers routinely screen, and a National Cancer Institute Community Oncology Research Program survey that showed 72% of respondents screened.
“Cancer centers are screening,” Lapen said. “The issue is turning that screening into action. I think a lot of centers don’t have the manpower and the resources; they may be limited on what they can feasibly do to help people given these constraints.”
Lapen highlighted strategies that have been effective at Memorial Sloan Kettering, including ride vouchers, which help patients better adhere to treatment, and referrals to financial navigators.
“Even when we were offering these services, only about 30% of patients that were flagged as being at risk accepted a referral for financial counseling services,” Lapen said.
Understanding uptake should be a significant focus of future research.
“We’re already bombarding patients with so much information in terms of treatment education and symptom assessment, it’s just another piece of information that they might not be able to fully grasp if it’s given in the context of their medical recommendations,” Lapen said. “We need to look at how we can best address this problem, look at what interventions may work versus ones that may not. That’s where we should focus.”
Senior author Fumiko Chino, MD, assistant professor in breast radiation oncology at The University of Texas MD Anderson Cancer Center and Healio Women in Oncology Peer Perspective Board Member, told Healio the first step is discussing these issues directly with patients.

Fumiko Chino
“You will not find the person who needs help if you don’t ask,” Chino, who also was a founding lead of the Affordability Working Group at Memorial Sloan Kettering, said. “That is the whole purpose of screening. When you go into the hospital, they’re going to ask if you’ve had a fall in the last month. They’re going to ask you if you feel blue as a depression screen. I feel financial toxicity and essential-needs screening is so important to ask every single person. That’s how we actually start fighting some of these gaps in care and disparity.”
References:
For more information:
Fumiko Chino, MD, can be reached at fchino@mdanderson.org.
Kaitlyn Lapen, MD, can be reached at lapenk@mskcc.org.