Triage:
-3.06pm on Wednesday afternoon
-Cat 3 to acute bed. 2/52 of worsening SOB on exertion +dry cough. Postural drop with CDA.
-Observations: BP 116/65, HR 80, RR 24, sats 96% on room air, temp 35.9C
History
-2/52 exertional dyspnoea and slight cough. Pre-syncopal x2 today whilst attempting to ambulate. LUQ non pleuritic and non-positional
-left total hip replacement 3 months prior. Mobilising with a stick. Discharged on aspirin
– PMH: HTN, T2DM, Stable Angina. No history of heart failure or history of VTE. Non-smoker
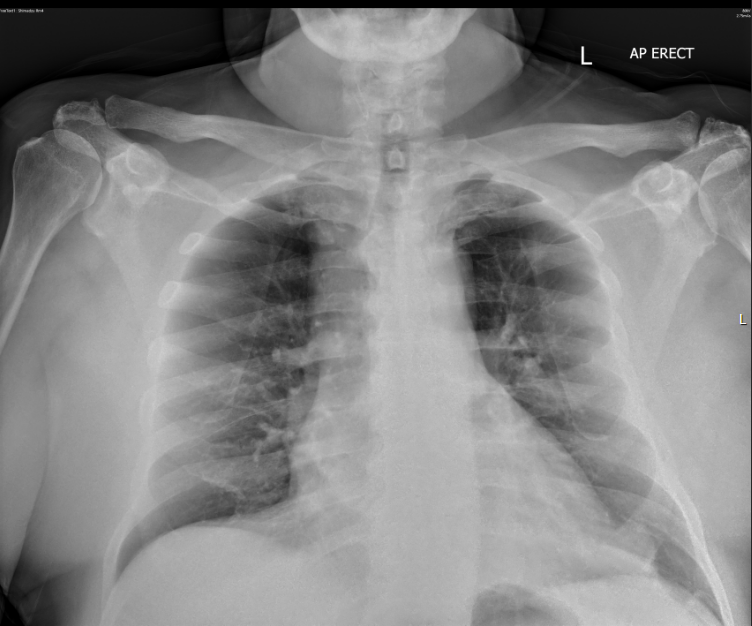
Chest Xray
A Point of Care ECHO (FELS) was performed.
PLAX:
How would you describe the heart in this view?
PSAX:
What’s the most obvious abnormality?
Subcostal 4CV and IVC:
What are the pertinent findings and the most likely diagnosis?
The cardinal echo features of PE on ultrasound are
What other features may be present ?
For further detailed information refer to https://www.criticalcare-sonography.com/2019/01/03/pulmonary-embolism-a-critical-care-echo-skill/
Progress:
Findings relayed to treating ED team who were able to prioritise seeing patient and obtain urgent CTPA and respiratory consultation.
CTPA:
Multifocal large burden of occlusive and non-occlusive pulmonary embolus at the pulmonary trunk and main pulmonary arteries bilaterally. There are features of right heart strain on CT.
ECG:
RBBB. HR 102
Previous ECG 3 months prior had also shown RBBB so would not necessarily have pointed towards PE.
Progress:
-Started on heparin infusion, plan for low dose thrombolysis if further deterioration.
Transient hypotension to 79/60, however treated on heparin infusion only as recovered quickly.
-Formal echo next day:
dilated RV with impaired systolic function, severe tricuspid regurgitation, mild pulmonary hypertension, normal LV function.
-Lower limb doppler 6 days post admission showing L occlusive DVT popliteal and peroneal veins
-Flutter requiring amiodarone during inpatient stay
-Eventually discharged in 2 weeks on NOAC
Impact of point of care echo on patient care:
Immediate bedside diagnosis of likely PE and allowed grading (as patient had no history of lung disease or RV dysfunction)
Up triaged urgency of case and facilitated quicker CTPA
Facilitated faster admission decision and inpatient team review (respiratory, cardiology, ICU)
Take home points:
A point of care ECHO is often helpful in patients with a history of change in exercise tolerance or dyspnoea.
For any questions about the RPA ED COM or if you have any suitable cases please email Jay at jayashanki.perera@health.nsw.gov.au or Genevieve at genevieve.carbonatto@health.nsw.gov.au