Images Heimerich Bisterbosch
A 40 year old man presents with worsening abdominal distension on a background of alcoholic cirrhosis.
On examination:
- Cachectic
- Speaking in short sentences
- Tense abdominal distention from ascites
- Absent breath sound right chest
- Saturating 92% on 2l of oxygen
- BP 107/70
- HR 90/min
This is his chest Xray
There is a right hydrothorax.
An ECHO is performed to look for cardiac pathology.
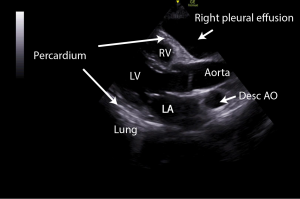
This is his PLAX
There is no pericardial effusion but there is a large right pleural effusion which can be seen overlying the right ventricle anteriorly.
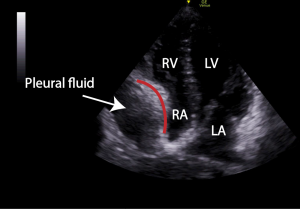
This is his 4 chamber view
The pleural effusion is visible. There is RA wall collapse and compression of the RA throughout the cardiac cycle. The RA wall collapse is worse every 6 or so beats most likely due increased intrapleural pressure on expiration.
A pleural drain was inserted and 2 litres of fluid was drained from the right hemithorax.
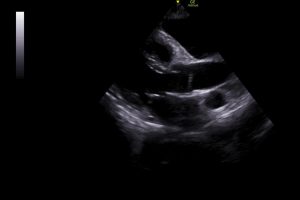
This is his post drainage ECHO
The RA is now expanding normally. There is still a significant pleural effusion that has not been completely drained.
Discussion:
Normal resting RAP is between 1-7 mmHg. Intrapericardial pressures vary with respiration between -4 ( on inspiration ) and +4 mmHg (on expiration) and are similar to the intrapleural pressure. With a pericardial effusion, intrapericardial pressures increase. With a pleural effusion, intrapleural pressures increase. In the case of a pleural effusion, increased intrapleural pressures are transmitted to the pericardium so the effect of a significant pleural effusion is similar on the heart to that of a pericardial effusion.
In pericardial effusion, the first sign of pre tamponade is right atrial (RA) wall collapse. This occurs when the RA pressure is at it’s lowest which is in early systole and intrapericardial pressures exceed RA pressures. The length of the RA wall collapse during the cardiac cycle is important. If it is collapsed for more than 1/3 of the cardiac cycle then this will have an effect on RV filling.
This patient had a pleural effusion and significant ascites.
RA wall collapse is due to the high intrapleural pressures from the large pleural effusion . This is further exacerbated by reduced RA filling due to this patient’s high intra abdominal pressures from his severe ascites. With ascites, the increased intra- abdominal hydrostatic pressure acts on the diaphragm affecting intrathoracic pressure impeding venous return to the RA.
After drainage of 2 l of fluid from this patient’s chest, there was complete resolution of the RA wall collapse.
This case highlights the importance of considering the impact of pleural fluid on the heart in the context of a patient with a pericardial effusion. Where there is a co existing pericardial effusion, a pleural effusion will compound the effect of the pericardial effusion on intracardiac pressures possibly leading to tamponade.
Drainage of a pleural effusion will decompress the thorax and may reverse tamponade physiology in a patient with a coexistant pericardial effusion.